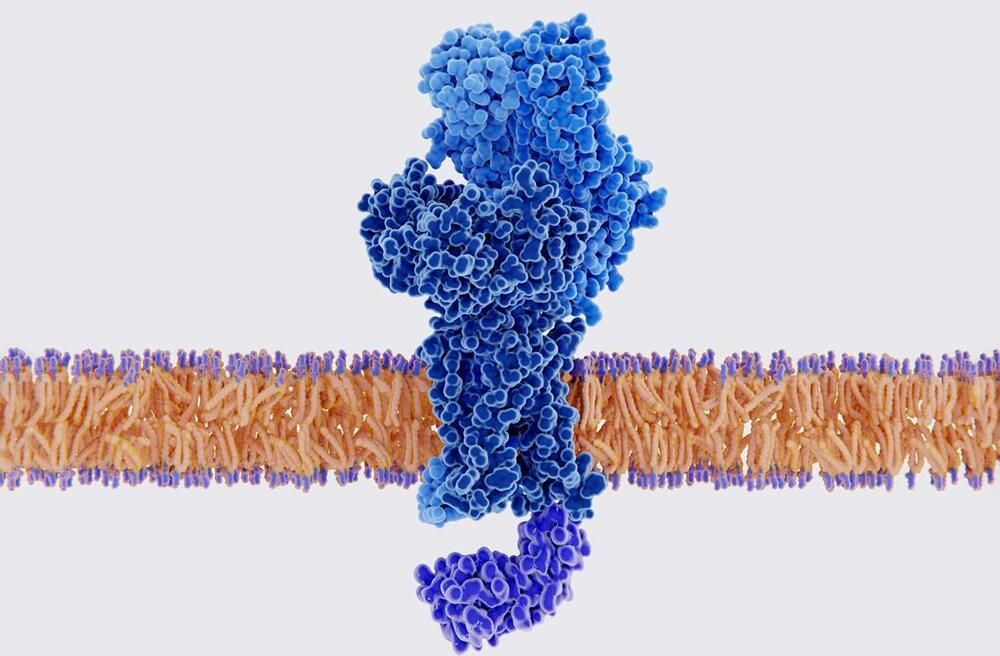
For the first time, an artificial molecular motor has been created that can ‘talk’ to living cells – by gently pulling their surface with enough physical force to elicit a biochemical response. The approach could help scientists decode the language that cells use to communicate with each other in tissues.
‘There is a mechanical language in the form of physical forces applied by the cells themselves, and we want to understand what information is communicated and what the consequences are,’ explains Aránzazu del Campo, who led the study at the Leibniz Institute for New Materials, Germany. ‘Ultimately, we want to be able to provide signals to cells and guide their function when they are not able to do that by themselves in disease cases.’
Usually, studying how cells communicate by sensing mechanical stimuli and producing biochemical responses requires prodding them with pipettes or the tip of an atomic force microscope. However, this doesn’t work at the more complex tissue level.