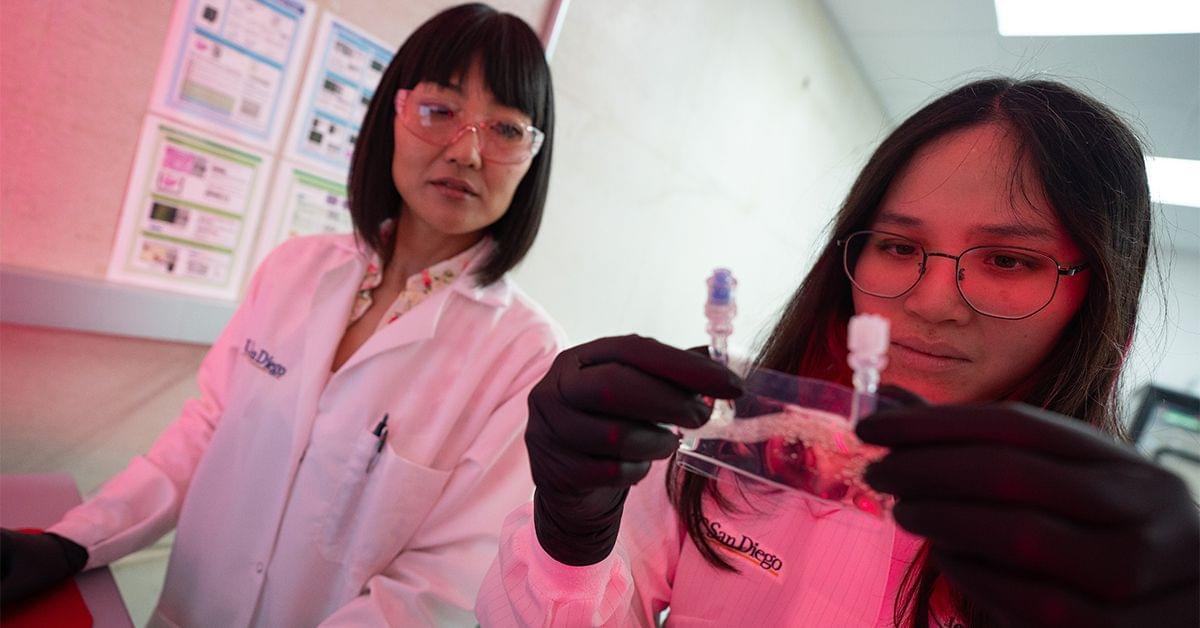
A new cancer treatment discovered by the University of California San Diego Sanford Stem Cell Institute (SSCI) and developed by Aspera Biomedicines will undergo testing in outer space this spring — this as researchers prepare to launch a clinical trial of the drug on Earth.
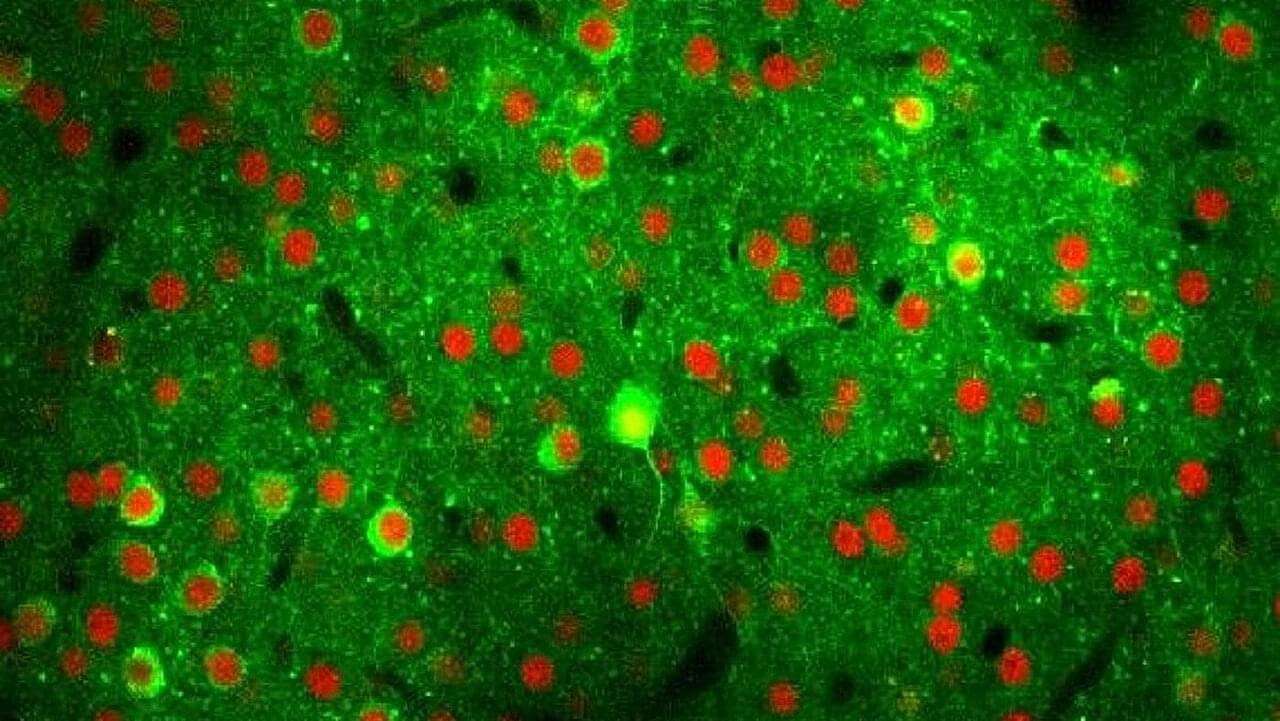
Rebecsinib, an investigational cancer drug slated to begin a Phase 1 clinical trial this year for patients with high-risk myelofibrosis or secondary acute myeloid leukemia, will be tested aboard the International Space Station (ISS) on four of the deadliest cancer types: ovarian cancer, metastatic breast cancer, acute myeloid leukemia and glioblastoma multiforme.
June 12, 2025
Rebecsinib, a new cancer treatment discovered by UC San Diego Sanford Stem Cell Institute will undergo testing in outer space on an additional four of the deadliest cancer types: ovarian cancer, metastatic breast cancer, acute myeloid leukemia and glioblastoma multiforme.