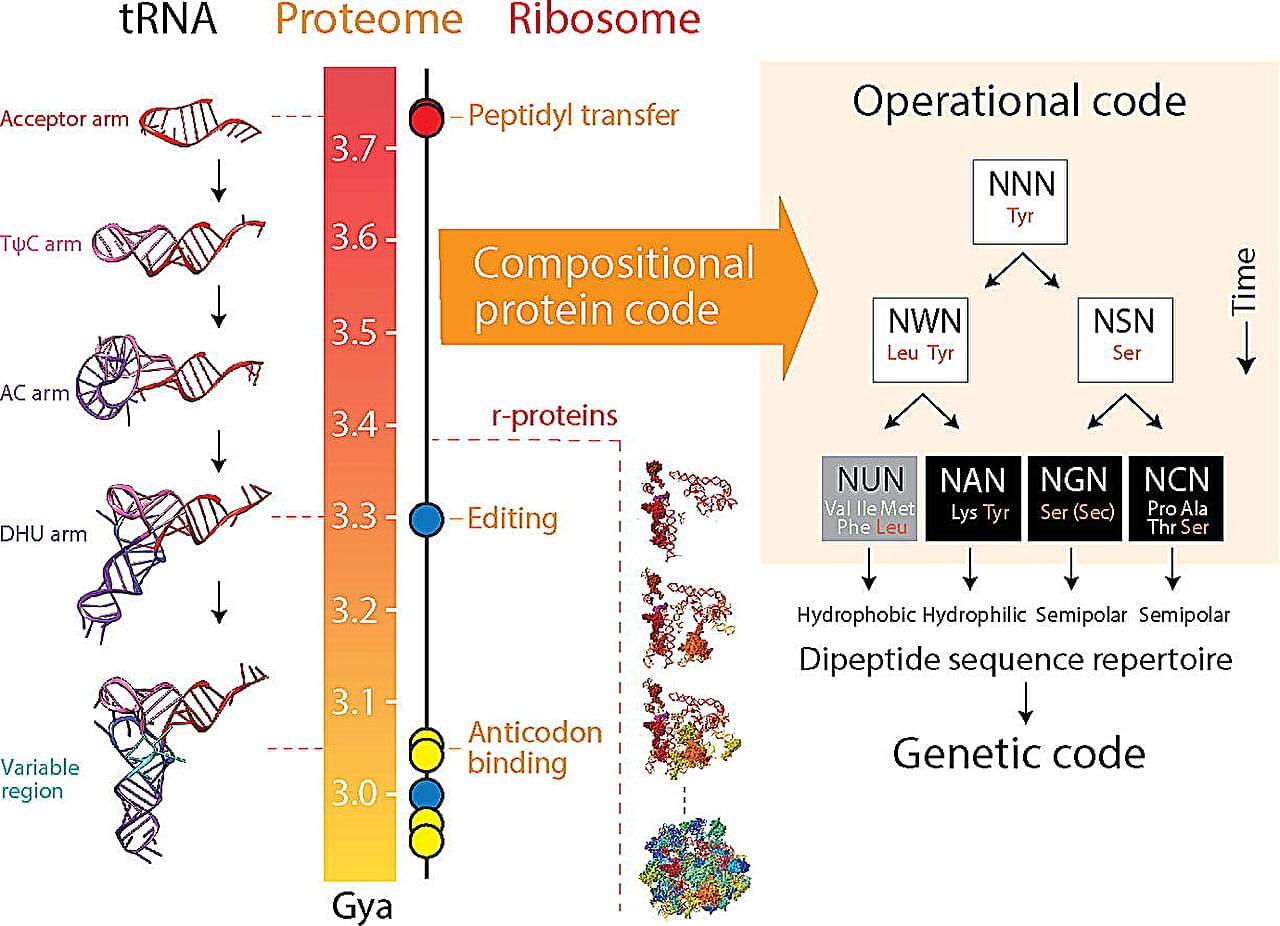
Genes are the building blocks of life, and the genetic code provides the instructions for the complex processes that make organisms function. But how and why did it come to be the way it is?
A recent study from the University of Illinois Urbana-Champaign sheds new light on the origin and evolution of the genetic code, providing valuable insights for genetic engineering and bioinformatics. The study is published in the Journal of Molecular Biology.
“We find the origin of the genetic code mysteriously linked to the dipeptide composition of a proteome, the collective of proteins in an organism,” said corresponding author Gustavo Caetano-Anollés, professor in the Department of Crop Sciences, the Carl R. Woese Institute for Genomic Biology, and Biomedical and Translation Sciences of Carle Illinois College of Medicine at U. of I.