Dr_Microbe/iStock.
Called Upstaza, the therapy not only improved the symptoms of all participants in the small-scale trial but also gave some children the ability to walk and talk for the first time.

The Indian Institute of Technology (IIT) Madras has announced a collaborative study with the Jet Propulsion Laboratory (JPL), the research hub of central US space agency National Aeronautics and Space Administration (NASA), to study the impact of microorganisms aboard the International Space Station. Observations from the research project will help create medical solutions to aid astronauts in long term human missions in space.
Explaining the observations, Karthik Raman, assistant professor at the department of biotechnology, IIT Madras, said that the collection of microbes, which includes a variety of bacteria and fungi, have occurred over time due to the astronauts that have been aboard the ISS over the past decades.
“Even though the ISS is a highly sterile environment, these microbes can play a big role in the way human presence in a space environment works — which our research work sought to highlight,” Raman said.

Gas stoves in California homes are leaking cancer-causing benzene, researchers found in a new study published on Thursday, though they say more research is needed to understand how many homes have leaks.
In the study, published in Environmental Science and Technology on Thursday, researchers also estimated that over 4 tons of benzene per year are being leaked into the atmosphere from outdoor pipes that deliver the gas to buildings around California — the equivalent to the benzene emissions from nearly 60,000 vehicles. And those emissions are unaccounted for by the state.
The researchers collected samples of gas from 159 homes in different regions of California and measured to see what types of gases were being emitted into homes when stoves were off. They found that all of the samples they tested had hazardous air pollutants, like benzene, toluene, ethylbenzene and xylene (BTEX), all of which can have adverse health effects in humans with chronic exposure or acute exposure in larger amounts.
Harnessing The Power Of Science & Innovation For All — Dr. Anna Laura Ross, Ph.D., Unit Head for Emerging Technologies, Research Prioritization and Support, Science Division, WHO.
Dr. Anna Laura Ross, Ph.D. is the Unit Head for Emerging Technologies, Research Prioritization and Support, in the World Health Organization (WHO) Science Division (https://www.who.int/our-work/science-division), located in Geneva, as well as the Head of the WHO Science Council Secretariat.
Previously at WHO, Dr Ross served as Strategy Technical Manager at Unitaid, their global health initiative that works with partners to bring about innovations to prevent, diagnose and treat major diseases in low-and middle-income countries, with an emphasis on tuberculosis, malaria, and HIV/AIDS and its deadly co-infections, providing strategic and technical support for Unitaid’s strategy, and working to identify the priorities areas for intervention to accelerate innovation for global health.
Dr. Ross has over fifteen years of experience in global health. Her areas of interest are in the field of HIV biomedical research, scientific program coordination, implementation research, and global health policy.
Prior to joining WHO, Dr. Ross served as Head of International Affairs and Scientific Relations at the National Agency for Research on AIDS and Viral Hepatitis (ANRS) in Paris, France.
A collaborative research team co-led by City University of Hong Kong (CityU) has developed a wearable tactile rendering system, which can mimic the sensation of touch with high spatial resolution and a rapid response rate.
The team demonstrated its application potential in a braille display, adding the sense of touch in the metaverse for functions such as virtual reality shopping and gaming, and potentially facilitating the work of astronauts, deep-sea divers and others who need to wear thick gloves.
“We can hear and see our families over a long distance via phones and cameras, but we still cannot feel or hug them. We are physically isolated by space and time, especially during this long-lasting pandemic,” said Dr. Yang Zhengbao, Associate Professor in the Department of Mechanical Engineering of CityU, who co-led the study.
(http://www.pharma.unizg.hr/en/about-us/staff/gordan–lauc, 450.html) is Professor of Biochemistry and Molecular Biology at the University of Zagreb, Faculty of Pharmacy and Biochemistry, and Founder and CEO of Genos Ltd. (https://genos-glyco.com/), a research-intensive SME located in Zagreb, Croatia with core of expertise in molecular genetics and glycomics (The comprehensive study the entire complement of sugars, whether free or present in more complex molecules of an organism) and they perform contract research, contract analysis and service for numerous universities, hospitals and private individuals in Europe and overseas.
Prof. Dr. Lauc also is CSO of GlycanAge LTD (https://glycanage.com/), a company that has developed a ground-breaking test that analyses your personal glycobiome for insights in improving your health and monitoring your biological age, and Co-Director of the Human Glycome Project (https://human-glycome.org/).
Prof. Dr. Lauc graduated with a degree in molecular biology at the University of Zagreb Faculty of Science in 1992, and obtained Ph.D. in Biochemistry and the University of Zagreb in 1995. He got his postdoctoral training at the Institute for Medical Physics and Biophysics in Münster and Johns Hopkins University in Baltimore. Since 1993 he has been employed at the Faculty of Pharmacy and Biochemistry in Zagreb. Between 1998 and 2010 he was also part-time employed at the University of Osijek School of Medicine where he founded a DNA laboratory for the identification of war victims and also served as Vice-Dean for Science between 2001 and 2005.
Prof. Dr. Lauc is author of over 100 research papers published in international journals and six international patents. He was invited to lecture at numerous international conferences, elected for visiting professor at the Johns Hopkins University and in 2011 also inducted in the prestigious Johns Hopkins Society of Scholars. If 2012 he was appointed Honorary Professor at the University of Edinburgh and Adjunct Professor at the Edith Cowan University in Perth.
Prof. Dr. Lauc chaired a number of conferences, including the “European Science Foundation Exploratory Workshop on Glycoscience” which resulted in the creation of the “European Glycoscience Forum”.
Prof. Dr. Lauc was a chairman of the committee that prepared Croatian National Action plan for the increased investment in research in development (2007), and was a member of the National Science Council between 2009 and 2013 and also and President of the National Council for Natural Sciences. He is a President-elect of the International Glycoscience Organization and member of the Steering Committee of the European Glycoscience Forum.

A Brazilian study published in Scientific Reports shows that artificial intelligence (AI) can be used to create efficient models for genomic selection of sugarcane and forage grass varieties and predict their performance in the field on the basis of their DNA.
In terms of accuracy compared with traditional breeding techniques, the proposed methodology improved predictive power by more than 50%. This is the first time a highly efficient genomic selection method based on machine learning has been proposed for polyploid plants (in which cells have more than two complete sets of chromosomes), including the grasses studied.
Machine learning is a branch of AI and computer science involving statistics and optimization, with countless applications. Its main goal is to create algorithms that automatically extract patterns from datasets. It can be used to predict the performance of a plant, including whether it will be resistant to or tolerant of biotic stresses such as pests and diseases caused by insects, nematodes, fungi or bacteria, and or abiotic stresses such as cold, drought, salinity or insufficient soil nutrients.

Alzheimer’s disease is a brain disorder that slowly destroys memory and thinking skills and, eventually, the ability to carry out the simplest tasks. In most people with the disease — those with the late-onset type symptoms first appear in their mid-60s. In a study from Brigham and Women’s Hospital, scientists found a new contributor to Alzheimer’s disease.

With Executive Order 14028, a large regulatory push toward mandating the production of a software bill of materials (SBOM) began. As this new buzzword spreads, you’d think it was a miracle cure for securing the software supply chain. Conceptually, it makes sense — knowing what is in a product is a reasonable expectation. However, it is important to understand what exactly an SBOM is and whether or not it can objectively be useful as a security tool.
SBOMs are meant to be something like a nutrition label on the back of a grocery store item listing all of the ingredients that went into making the product. While there currently is no official SBOM standard, a few guideline formats have emerged as top candidates. By far, the most popular is the Software Data Package Exchange (SPDX), sponsored by the Linux Foundation.
SPDX, as with most other formats, attempts to provide a common way to represent basic information about the ingredients that go into the production of software: names, versions, hashes, ecosystems, ancillary data like known flaws and license information, and relevant external assets. However, software is not as simple as a box of cereal, and there is no equivalent to the Food and Drug Administration enforcing compliance to any recommended guidelines.
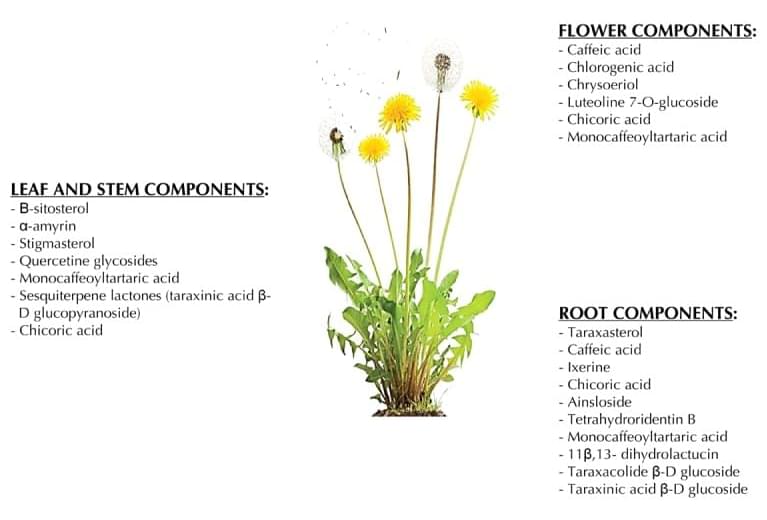
The tremendous rise in the economic burden of type 2 diabetes (T2D) has prompted a search for alternative and less expensive medicines. Dandelion offers a compelling profile of bioactive components with potential anti-diabetic properties. The Taraxacum genus from the Asteraceae family is found in the temperate zone of the Northern hemisphere. It is available in several areas around the world. In many countries, it is used as food and in some countries as therapeutics for the control and treatment of T2D. The anti-diabetic properties of dandelion are attributed to bioactive chemical components; these include chicoric acid, taraxasterol (TS), chlorogenic acid, and sesquiterpene lactones. Studies have outlined the useful pharmacological profile of dandelion for the treatment of an array of diseases, although little attention has been paid to the effects of its bioactive components on T2D to date. This review recapitulates previous work on dandelion and its potential for the treatment and prevention of T2D, highlighting its anti-diabetic properties, the structures of its chemical components, and their potential mechanisms of action in T2D. Although initial research appears promising, data on the cellular impact of dandelion are limited, necessitating further work on clonal β-cell lines (INS-1E), α-cell lines, and human skeletal cell lines for better identification of the active components that could be of use in the control and treatment of T2D. In fact, extensive in-vitro, in-vivo, and clinical research is required to investigate further the pharmacological, physiological, and biochemical mechanisms underlying the effects of dandelion-derived compounds on T2D.
Keywords: type 2 diabetes, dandelion, chlorogenic acid, chicory acid, taraxasterol, sesquiterpene.
Abbreviations: ADP — adenosine diphosphate; AFLD — alcoholic fatty liver disease; AMPK — adenosine monophosphate-activated protein kinase; ATP — adenosine triphosphate; cAMP — cyclic adenosine monophosphate; CGA — chlorogenic acid; CoA — coenzyme A; CRA — chicory acid; DAG — diacylglycerol; DBD — DNA-binding domain; DNA — deoxyribonucleic acid; DPPH — 2,2-diphenyl-1-picrylhydrazyl; Dw — dry weight; FOS — fructose oligosaccharide; G6P — glucose-6-phosphate; GDP — guanosine 5’-diphosphate; GLP-1 — glucagon-like peptide 1; GLUT2 — glucose transporter 2; GLUT4 — muscle glucose transporter protein 4; GPCR — G protein-coupled receptor; GTP — guanosine triphosphate; HNB — 2-hydroxy-5-nitrobenzenaledehyde; HPLC — high-pressure liquid chromatography; IC50 — half maximal inhibitory concentration; IDF — International Diabetes Federation; IDX-1 — islet duodenum homeobox 1; IL-1α — interleukin 1 alpha; INS-1E — rat insulinoma clonal beta-cell line; IR — insulin receptor; IRS-1 — insulin receptor substrate 1; Km — Michaelis constant; IP3 — inositol triphosphate; IRS-1 — insulin receptor substrate 1; LBD — ligand-binding domain; LC-DAD — liquid chromatography with (photo) diode array detection; LPS — lipopolysaccharide; MAPK — mitogen-activated protein kinase; NADH — nicotinamide adenine dinucleotide; NAFLD — non-alcoholic fatty liver disease; NF-κb — nuclear factor kappa B; NO — nitric oxide; PI3K — phosphatidylinositol 3 kinase; PKA — protein kinase A; PKC — protein kinase C; PPAR-γ — peroxisome proliferator-activated receptor gamma; ROS — reactive oxygen species; RxR — retinoid X receptor; SEL — sesquiterpene lactones; SUR1 — sulphonylurea receptor 1; T2D — type 2 diabetes; TAG — triacylglycerol; TNF-α — tumor necrosis factor; TO — Taraxacum officinale; TS — taraxasterol; UPLC-MS/MS — ultra-performance liquid chromatography — tandem mass spectrometry; UV/VIS — ultraviolet visible; WHO — World Health Organization.