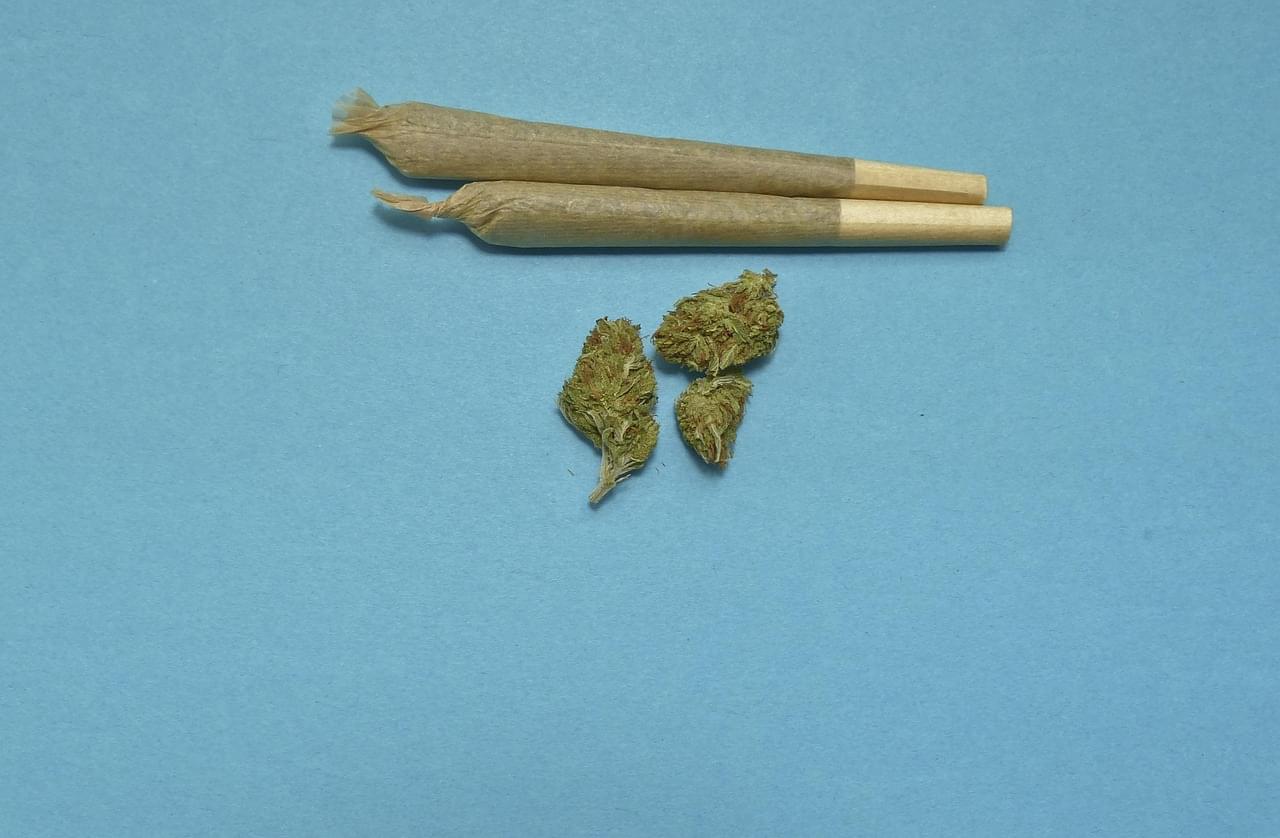
Rising cannabis use and falling smoking rates suggest legalization drives substitution of cannabis for cigarettes.
How does cannabis use influence cigarette smoking? This is what a recent study published in Addictive Behaviors hopes to address as a team of researchers investigated how recreational cannabis legalization has caused shifts in social dynamics, specifically regarding cigarette use. This study has the potential to help researcher better understand the social impacts of recreational cannabis legalization and the steps that can be taken to mitigate the negative impacts.
For the study, the researchers analyzed data obtained from the National Survey on Drug Use and Health for 30-day trends regarding cannabis-only use, cigarette-only use, and co-use for individuals 18 years and older and from time periods of 2015–2019, 2020, and 2021–2023. The goal of the study was to draw a connection between cannabis legalization and cigarette use, or co-use. In the end, the researchers found increases in cannabis-only use in 2015–2019, 2020, and 2021–2023 at 3.9% to 6.5%, 7.1%, and 7.9% to 10.6%, respectively. In contrast, cigarette-only use decreased during these same time periods at 15% to 12%, 10.3%, and 10.8% to 8.8%, respectively. Finally, the researchers observed consistent co-use during all three periods.
“The rising cannabis-only use across groups parallels the expanding state-level recreational cannabis legalization, increasing accessibility and normalization,” the study notes. “Conversely, continued declines in cigarette-only use align with decades of tobacco control efforts and evolving norms surrounding smoking. The relatively stable co-use trends may reflect substitution dynamics whereby some individuals replace cigarettes with cannabis, preventing co-use from rising in tandem with cannabis-only use.”