What happens to soft matter when gravity disappears? To answer this, UvA physicists launched a fluid dynamics experiment on a sounding rocket. The suborbital rocket reached an altitude of 267 km before falling back to Earth, providing six minutes of weightlessness.
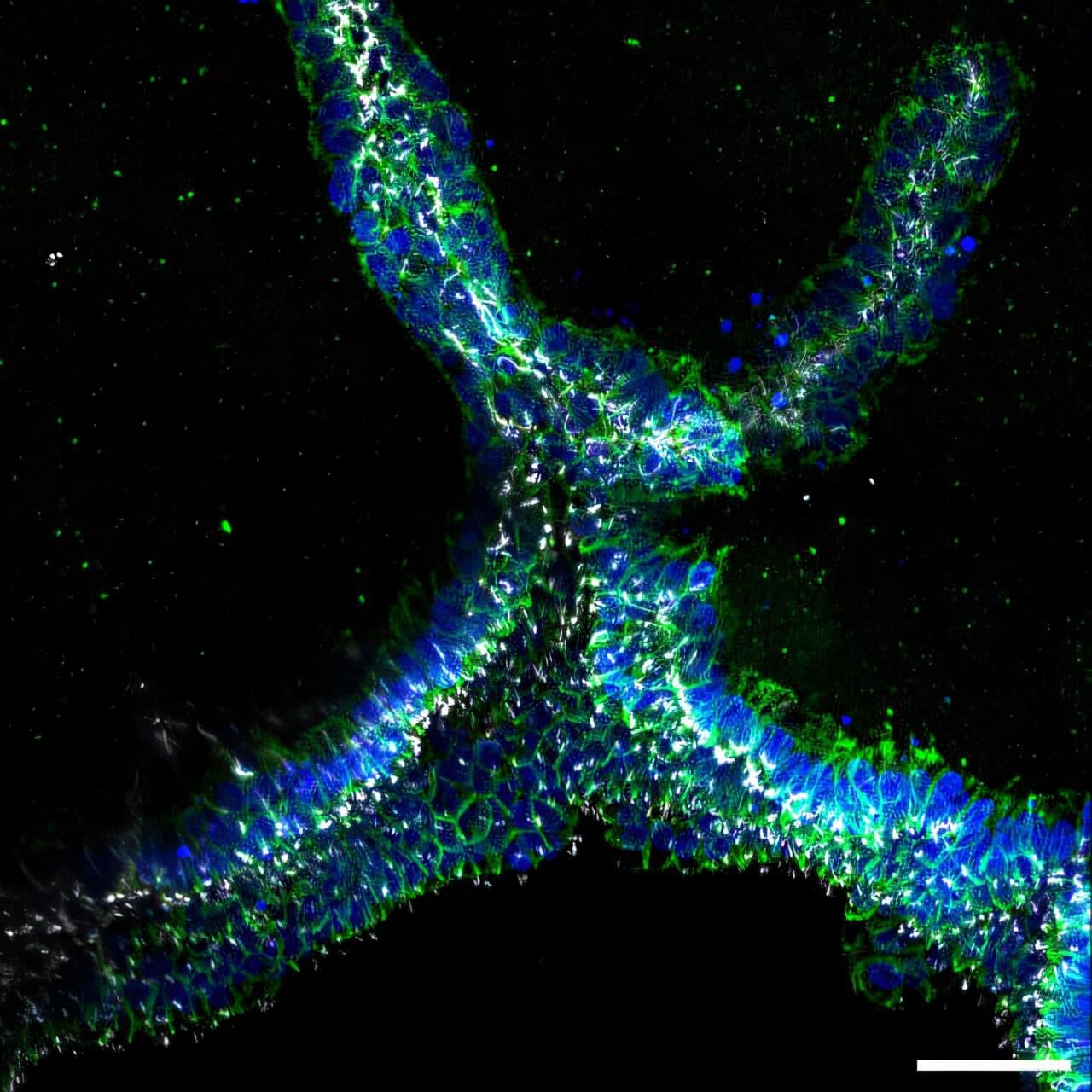
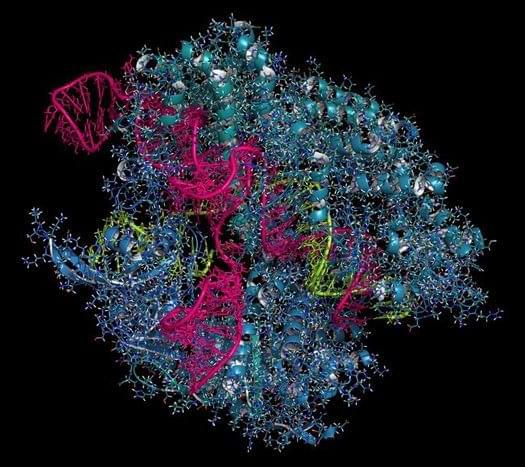
In these six minutes, the researchers 3D-printed large droplets of a soft material similar to the inks used for bioprinting —a developing technology that shows huge potential for regenerative and personalized medicine, tissue engineering and cosmetics. Bioprinting involves 3D-printing a mix of cells and bio-inks or bio-materials in a desired shape, often to construct living tissues.
The experiment was called COLORS (COmplex fluids in LOw gravity: directly observing Residual Stresses). Using a special optical set-up, the researchers could see where the printed material experienced internal stresses (forces) as the droplets spread and merged. Stressed regions stand out as bright colors in the experiment. Investigating how and where these stresses emerge is important because they can get frozen in a material as it solidifies, creating weak points where 3D-printed objects are most likely to break.