We live immersed in a persistent illusion: the idea that consciousness arises from the brain like the flame from a candle. Contemporary science, constrained by the very instruments it creates, proclaims that the mind is merely the result of electrical impulses and chemical reactions — an epiphenomenon of flesh.
Yet a deeper look — one that doesn’t reject science but rather transcends it — reveals a more radical reality: we, living beings, are not the origin of consciousness, but rather its antenna.
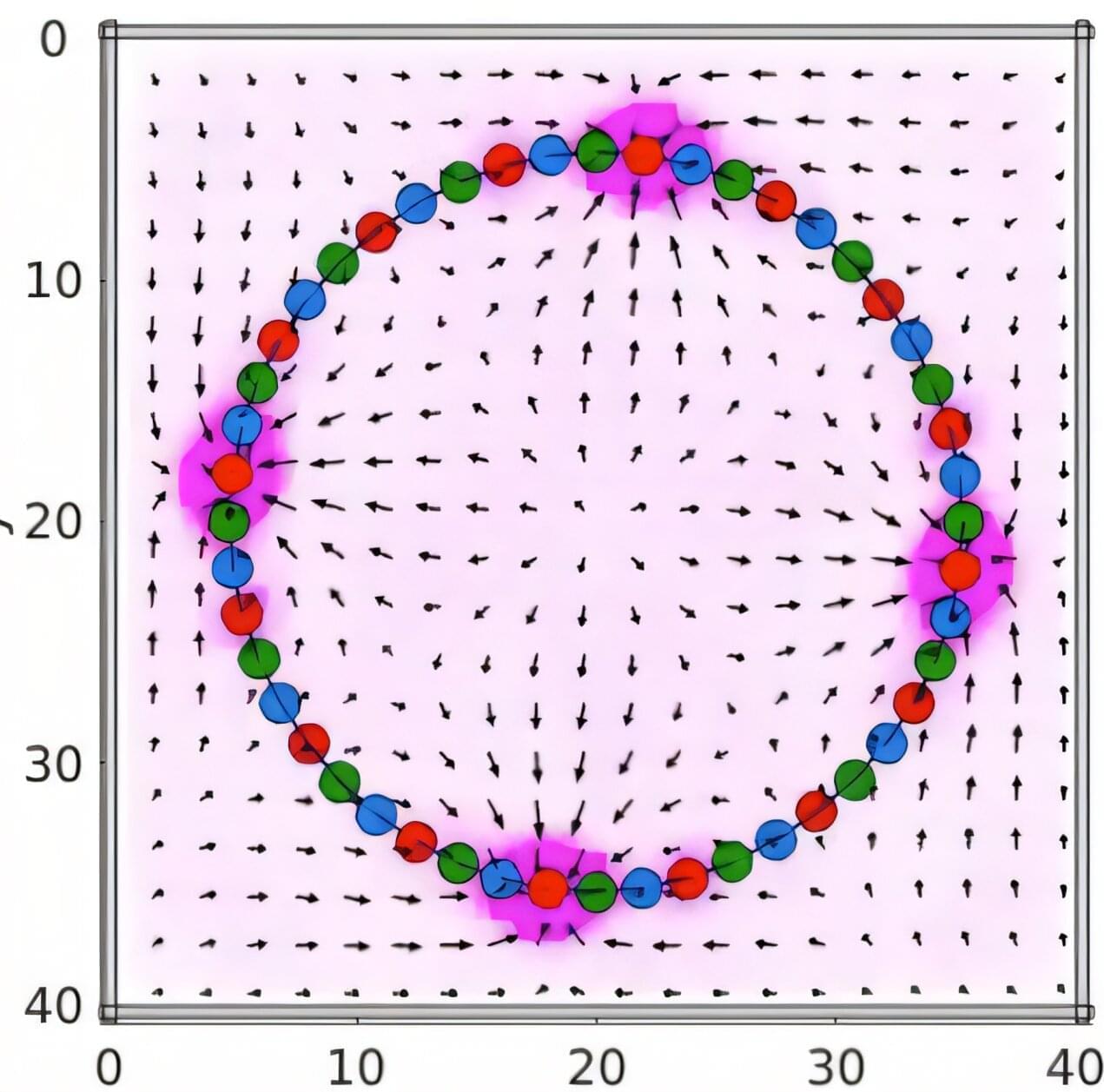
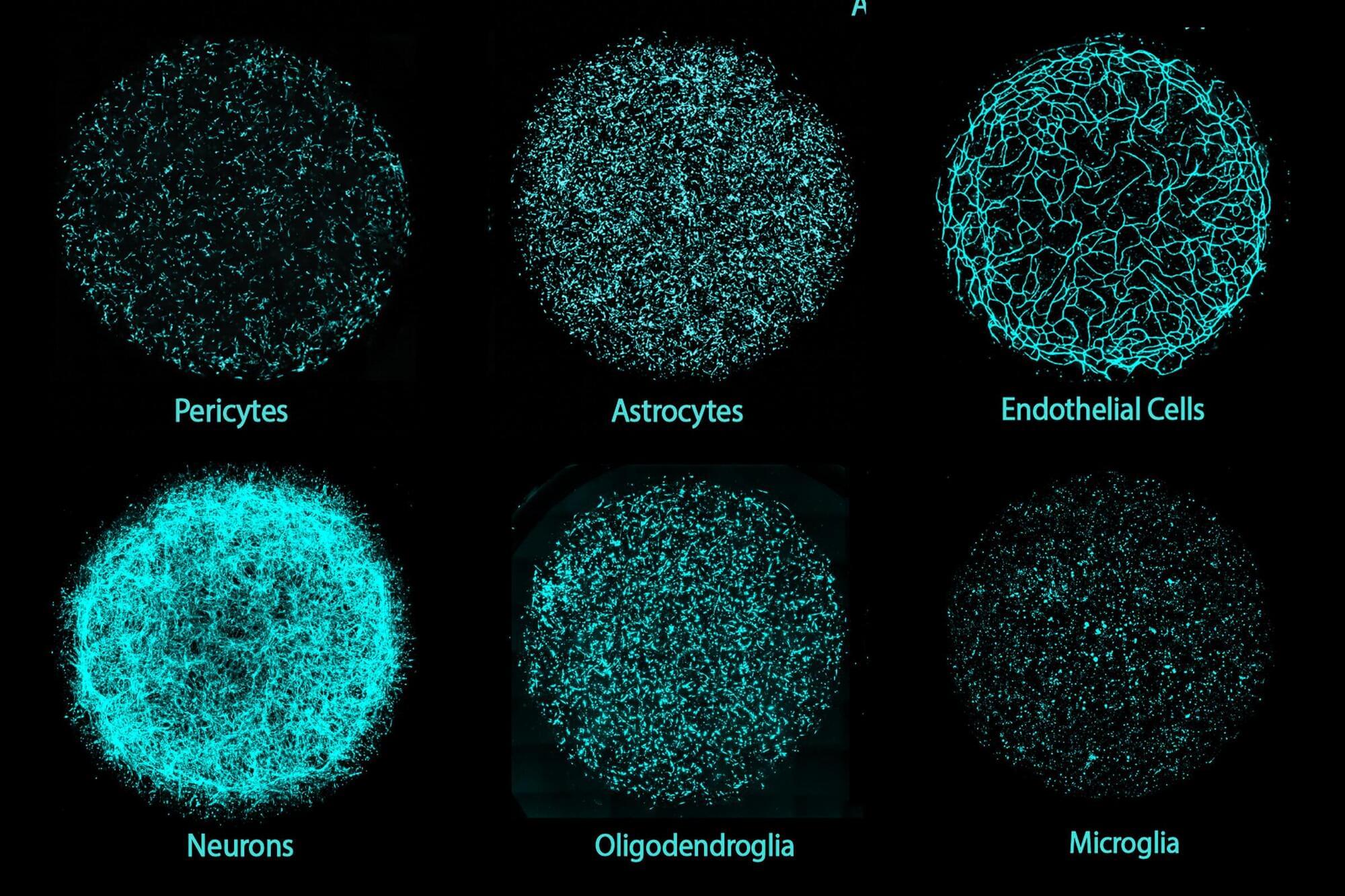
We are hardware. Bodies shaped by millions of years of biological evolution, a complex architecture of atoms and molecules organized into a fractal of systems. But this hardware, no matter how sophisticated, is nothing more than a receptacle, a stage, an antenna. What truly moves, creates, and inspires does not reside here, within this tangible three-dimensional realm; it resides in an unlimited field, a divine matrix where everything already exists. Our mind, far from being an original creator, is a channel, a receiver, an interpreter.
The great question of our time — and perhaps of all human history — is this: how can we update the software running on this biological hardware without the hardware itself becoming obsolete? Herein lies the fundamental paradox: we can dream of enlightenment, wisdom, and transcendence, yet if the body does not keep pace — if the physical circuits cannot support the flow — the connection breaks, the signal distorts, and the promise of spiritual evolution stalls.
The human body, a product of Darwinian evolution’s slow dance, is both marvel and prison. Our eyes capture only a minuscule fraction of the electromagnetic spectrum; our ears are limited to a narrow range of frequencies; our brains filter out and discard 99% of the information surrounding us. Human hardware was optimized for survival — not for truth!
This is the first major limitation: if we are receivers of a greater reality, our apparatus is radically constrained. It’s like trying to capture a cosmic symphony with an old radio that only picks up static. We may glimpse flashes — a sudden intuition, an epiphany, a mystical experience — but the signal is almost always imperfect.
Thus, every spiritual tradition in human history — from shamans to mystery schools, from Buddhism to Christian mysticism — has sought ways to expand or “hack” this hardware: fasting, meditation, chanting, ecstatic dance, entheogens. These are, in fact, attempts to temporarily reconfigure the biological antenna to tune into higher frequencies. Yet we remain limited: the body deteriorates, falls ill, ages, and dies.
If the body is hardware, then the mind — or rather, the set of informational patterns running through it — is software: human software (and a limited one at that). This software isn’t born with us; it’s installed through culture, language, education, and experience. We grow up running inherited programs, archaic operating systems that dictate beliefs, prejudices, and identities.
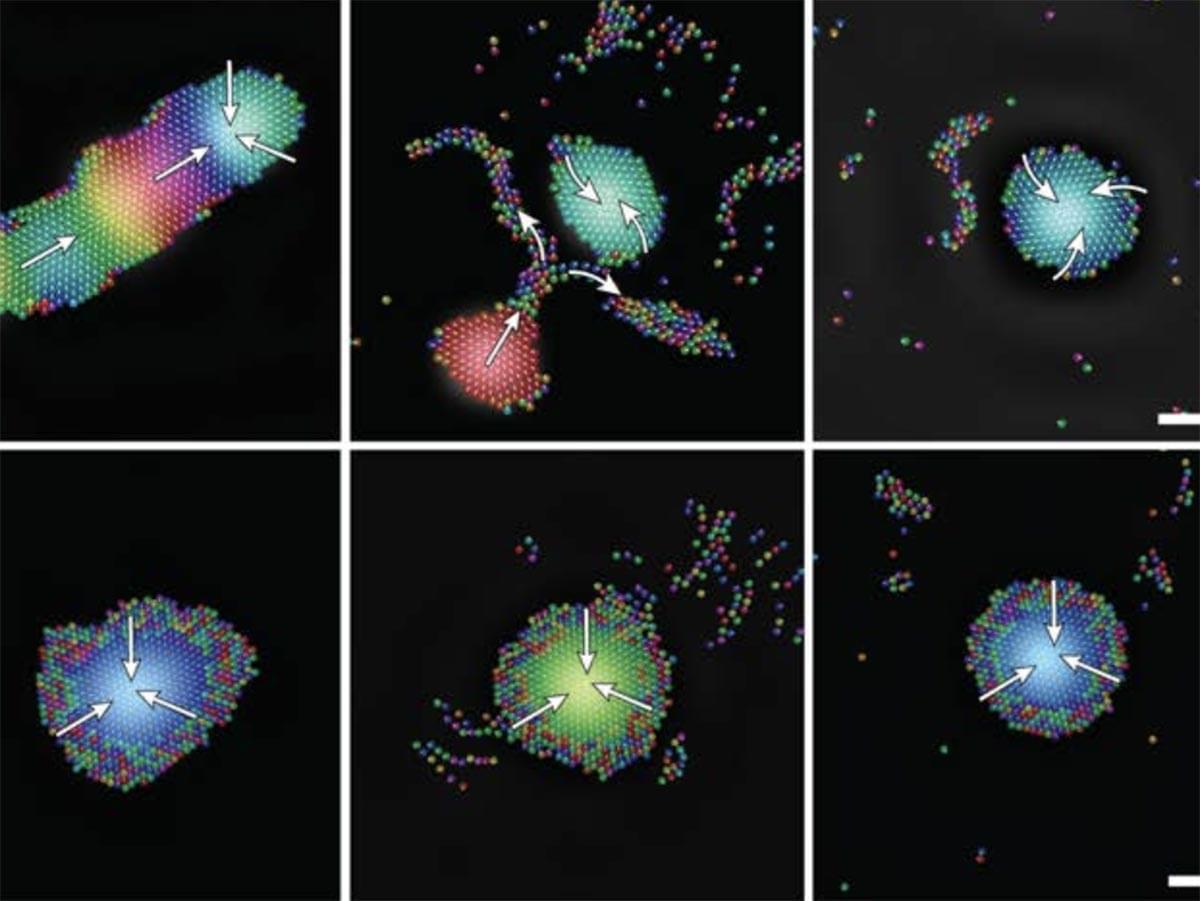
Beneath this cultural software, however, lies a deeper code: access to an unlimited field of possibilities. This field — call it God, Source, Cosmic Consciousness, the Akashic Records, it doesn’t matter — contains everything: all ideas, all equations, all music, all works of art, all solutions to problems not yet conceived. We don’t invent anything; we merely download it.
Great geniuses throughout history — from Nikola Tesla to Mozart, from Leonardo da Vinci to Fernando Pessoa — have testified to this mystery: ideas “came” from outside, as if whispered by an external intelligence. Human software, then, is the interface between biological hardware and this divine ocean. But here lies the crucial question: what good is access to supreme software if the hardware lacks the capacity to run it?
An old computer might receive the latest operating system, but only if its minimum specifications allow it. Otherwise, it crashes, overheats, or freezes. The same happens to us: we may aspire to elevated states of consciousness, but without a prepared body, the system fails. That’s why so many mystical experiences lead to madness or physical collapse.
Thus, we arrive at the heart of the paradox. If the hardware doesn’t evolve, even the most advanced software download is useless. But if the software isn’t updated, the hardware remains a purposeless machine — a biological robot succumbing to entropy.
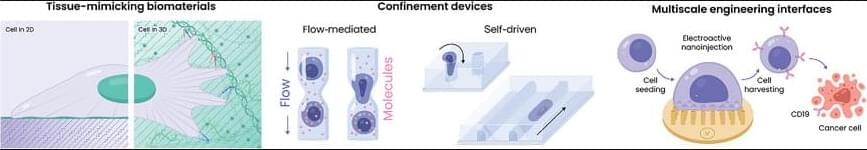
Contemporary society reflects this tension. On one hand, biotechnology, nanotechnology, and regenerative medicine promise to expand our hardware: stronger, more resilient, longer-lived bodies. On the other, the cultural software governing us remains archaic: nationalism, tribalism, dogma, consumerism. It’s like installing a spacecraft engine onto an ox-drawn cart.
At the opposite end of the spectrum, we find the spiritual movement, which insists on updating the software — through meditation, energy therapies, expanded states of consciousness — but often neglects the hardware. Weakened, neglected bodies, fed with toxins, become incapable of sustaining the frequency they aim to channel. The result is a fragile, disembodied spirituality — out of sync with matter.
Humanity’s challenge in the 21st century and beyond is not to choose between hardware and software, but to unify them. Living longer is meaningless if the mind remains trapped in limiting programs. Aspiring to enlightenment is futile if the body collapses under the intensity of that light.
It’s essential to emphasize: the power does not reside in us (though, truthfully, it does — if we so choose). This isn’t a doctrine of self-deification, but of radical humility. We are merely antennas. True power lies beyond the physical reality we know, in a plane where everything already exists — a divine, unlimited power from which Life itself emerges.
Our role is simple yet grand: to invoke. We don’t create from nothing; we reveal what already is. We don’t invent; we translate. A work of art, a mathematical formula, an act of compassion — all are downloads from a greater source.
Herein lies the beauty: this field is democratic. It belongs to no religion, no elite, no dogma. It’s available to everyone, always, at any moment. The only difference lies in the hardware’s capacity to receive it and the (human) software that interprets it.
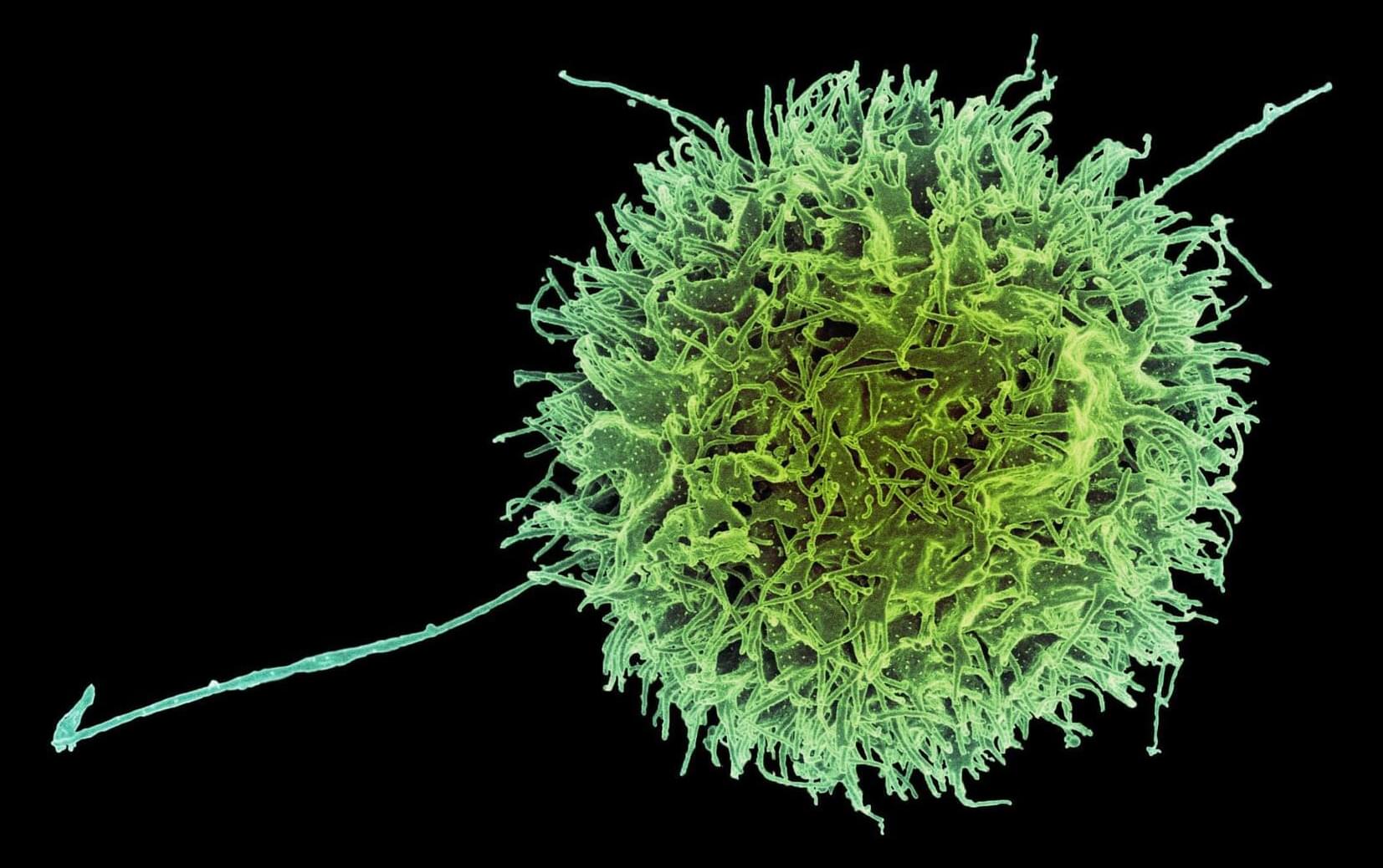
But there are dangers. If the hardware is weak or the software corrupted, the divine signal arrives distorted. This is what we see in false prophets, tyrants, and fanatics: they receive fragments of the field, but their mental filters — laden with fear, ego, and the desire for power — twist the message. Instead of compassion, violence emerges; instead of unity, division; instead of wisdom, dogma.
Therefore, conscious evolution demands both purification of the software (clearing toxic beliefs and hate-based programming) and strengthening of the hardware (healthy bodies, resilient nervous systems). Only then can the divine frequency manifest clearly.
If we embrace this vision, humanity’s future will be neither purely biological nor purely spiritual — it will be the fusion of both. The humans of the future won’t merely be smarter or longer-lived; they’ll be more attuned. A Homo Invocator: the one who consciously invokes the divine field and translates it into matter, culture, science, and art.
The initial paradox remains: hardware without software is useless; software without hardware is impossible. But the resolution isn’t in choosing one over the other — it’s in integration. The future belongs to those who understand that we are antennas of a greater power, receivers of an infinite Source, and who accept the task of refining both body and mind to become pure channels of that reality.
If we succeed, perhaps one day we’ll look back and realize that humanity’s destiny was never to conquer Earth or colonize Mars — but to become a conscious vehicle for the divine within the physical world.
And on that day, we’ll understand that we are neither merely hardware nor merely software. We are the bridge.
Deep down, aren’t we just drifting objects after all?
The question is rhetorical, for I don’t believe any of us humans holds the answer.
__
Copyright © 2025, Henrique Jorge (ETER9)
Image by Gerd Altmann from Pixabay
[ This article was originally published in Portuguese in Link to Leaders at: https://linktoleaders.com/o-ser-como-interface-henrique-jorge-eter9/]