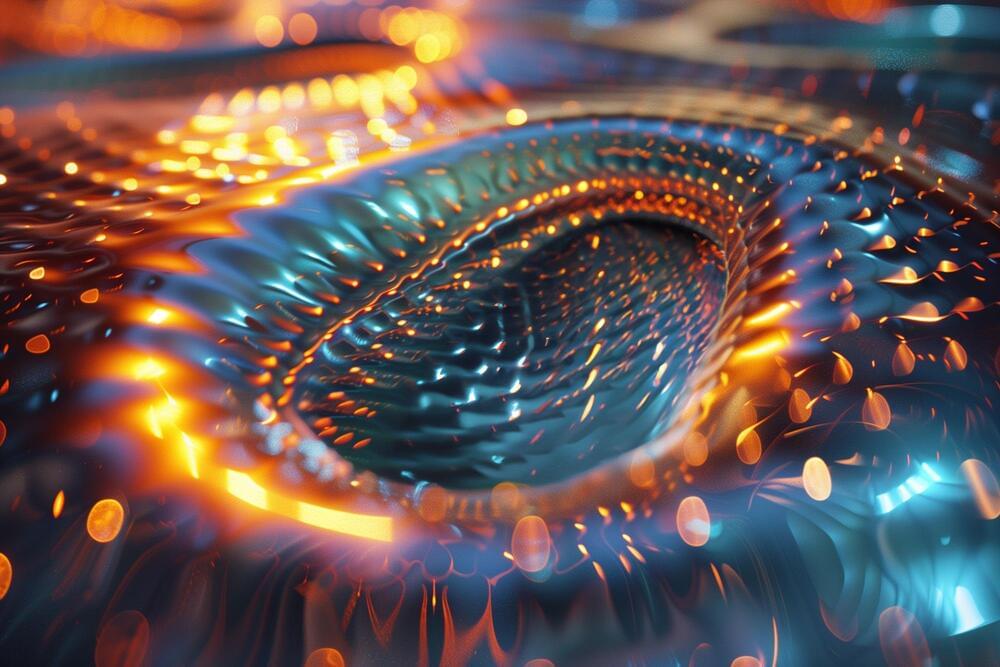
In a breakthrough, scientists confirmed superfluid properties in supersolids by observing quantized vortices. Using precision techniques, the team stirred a rotating supersolid, revealing unique vortex dynamics and offering new insights into the coexistence of solid and fluid characteristics. This discovery paves the way for studying exotic quantum matter and has implications for astrophysical phenomena.
Supersolids: A Quantum Paradox
Matter that behaves like both a solid and a superfluid at the same time might sound impossible. But more than 50 years ago, physicists predicted that quantum mechanics could allow such a state. In this unique state, collections of particles exhibit properties that seem contradictory. Francesca Ferlaino from the Department of Experimental Physics at the University of Innsbruck and the Institute of Quantum Optics and Quantum Information (IQOQI) at the Austrian Academy of Sciences explains, “It is a bit like Schrödinger’s cat, which is both alive and dead, a supersolid is both rigid and liquid.”