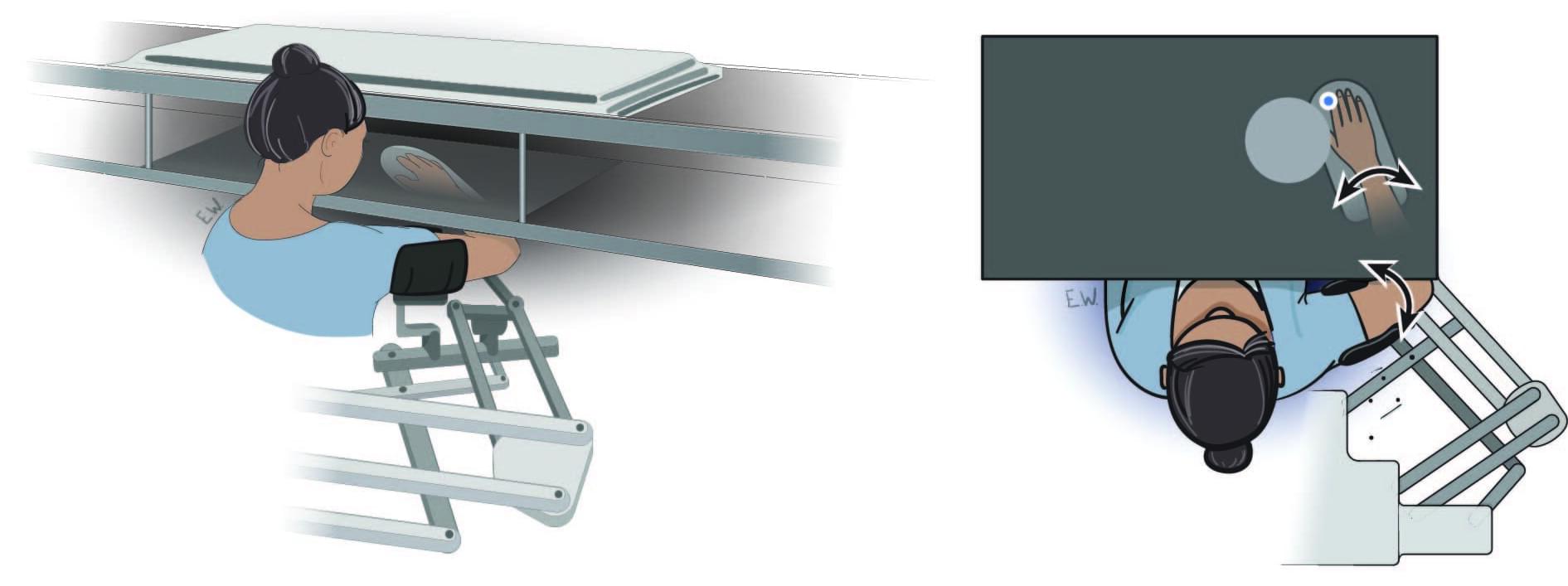
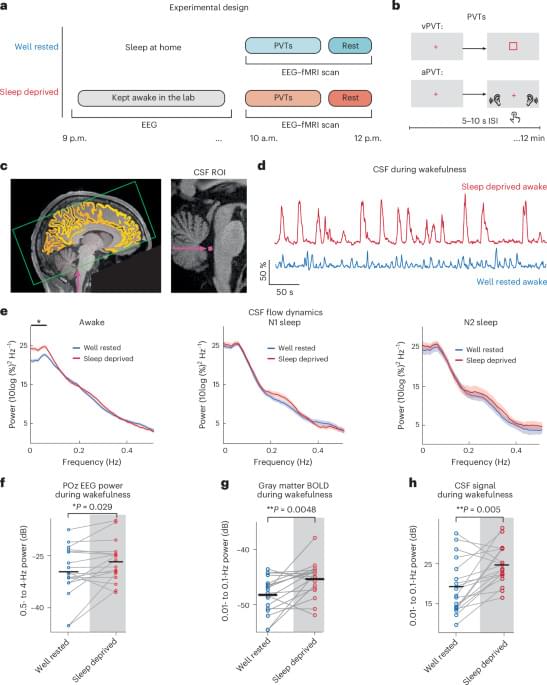
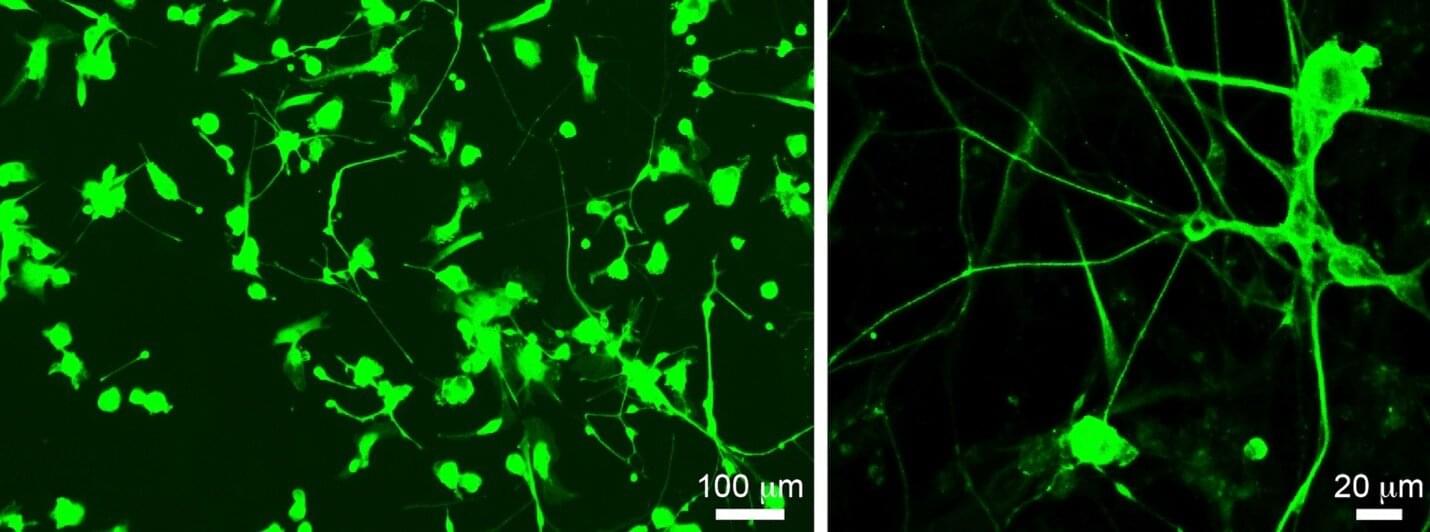
A study led by Jonathan Michaels, a Faculty of Health professor at York’s School of Kinesiology and Health Science, reveals how the brains of humans and monkeys use sensory expectations to prepare for unexpected disturbances, enabling faster and more accurate motor responses.
Published today in Nature, the study demonstrates that motor circuits across the brain do not passively wait for sensory signals. Instead, they proactively anticipate potential challenges, configuring themselves to respond effectively to disturbances. The research represents a significant leap forward in uncovering the brain’s predictive capabilities and its role in motor control.
This advancement provides a clearer picture of the neural mechanisms underlying movement preparation and response, illustrating how expectation itself enhances precision and stability. The discovery opens new pathways for improving rehabilitation techniques and advancing brain-computer interface technology.