To learn to socialize, zebrafish need to trust their gut.
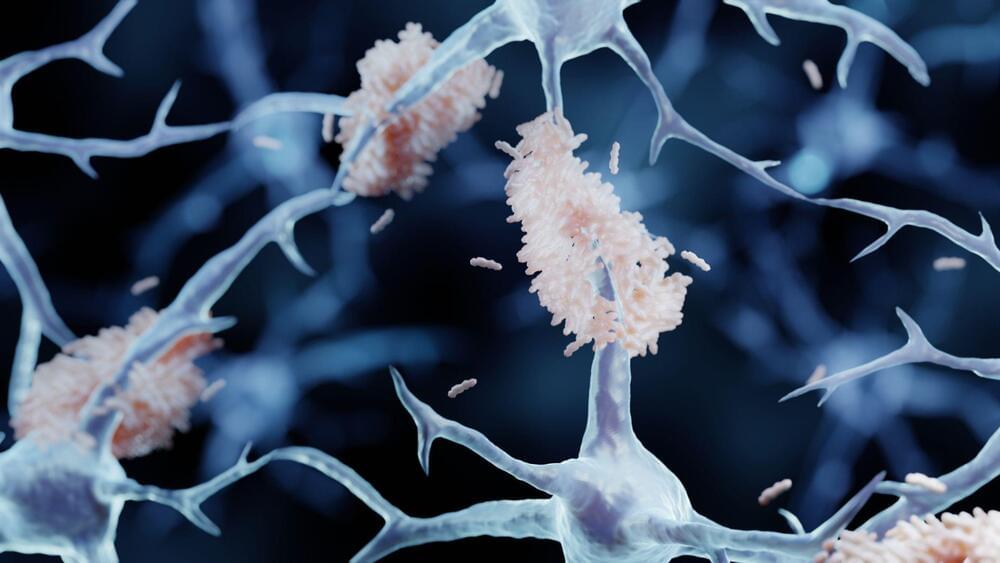
Gut microbes encourage specialized cells to prune back extra connections in brain circuits that control social behavior, new University of Oregon research in zebrafish shows. The pruning is essential for the development of normal social behavior.
The researchers also found that these ‘social’ neurons are similar in zebrafish and mice. That suggests the findings might translate between species — and could possibly point the way to treatments for a range of neurodevelopmental conditions.