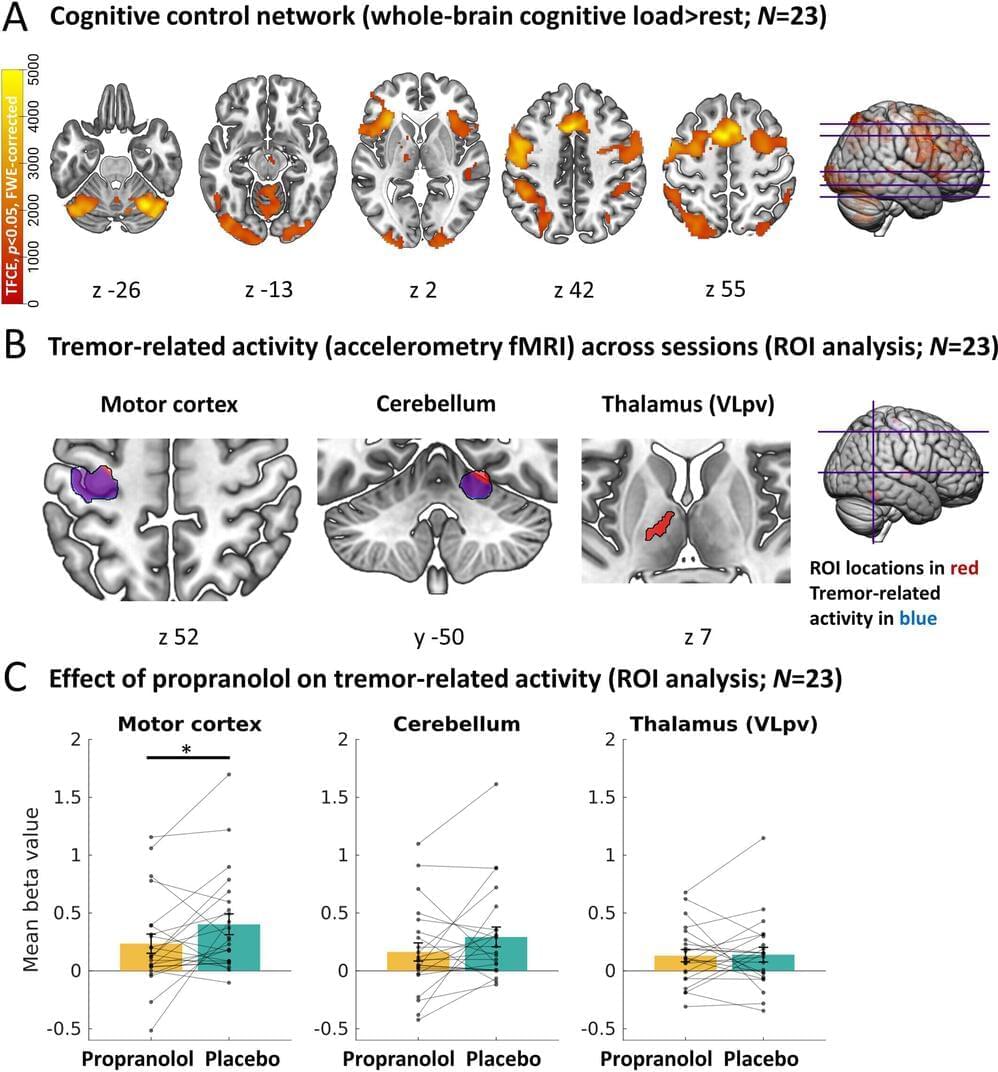
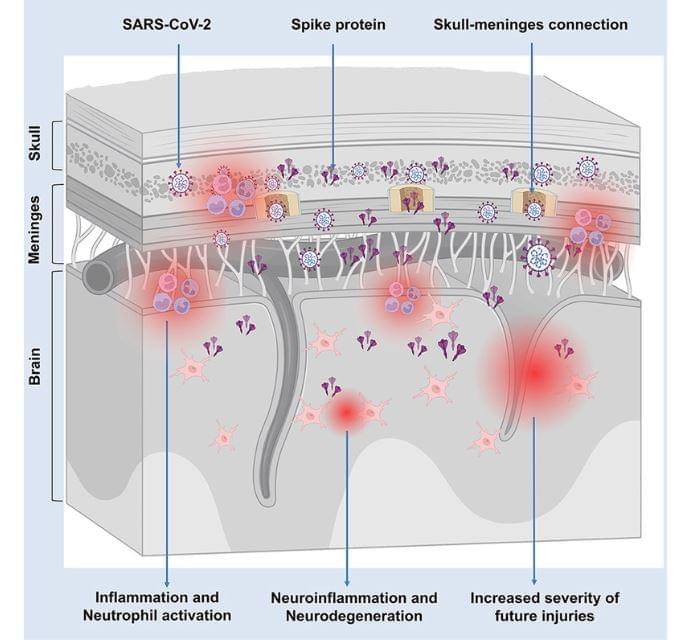
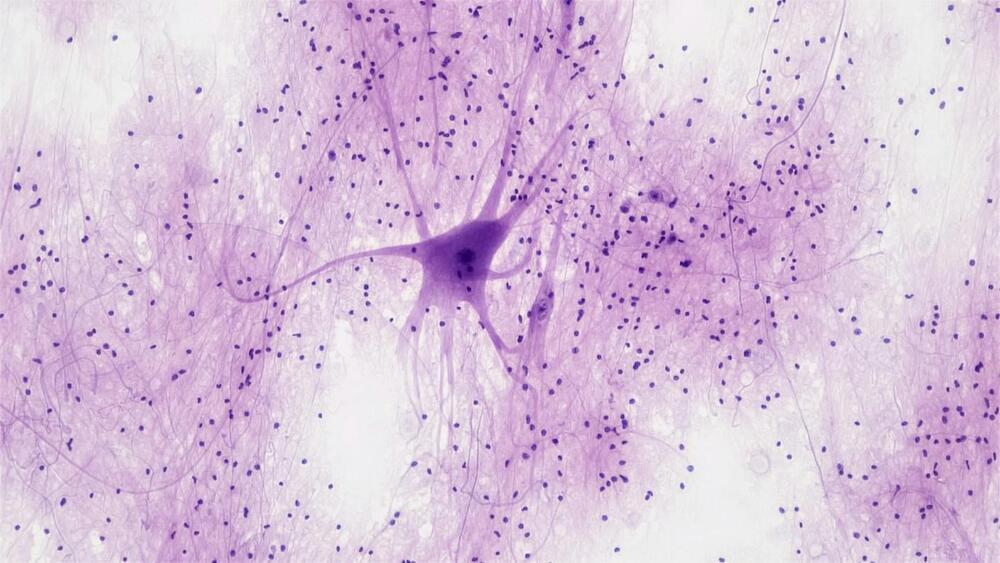
The standard medication levodopa does not always work against tremors in Parkinson’s disease, especially in stressful situations. Propranolol, however, does work during stress, providing insight into the role of the stress system in tremors. MRI scans reveal that propranolol directly inhibits activity in the brain circuit that controls tremors. Doctors may consider this medication when levodopa is ineffective.
People with Parkinson’s disease report that tremors worsen during stressful situations. “Tremors act as a sort of barometer for stress; you see this in all people with Parkinson’s,” says neurologist Rick Helmich from Radboud university medical center.
The commonly used drug levodopa usually helps with tremors, but it tends to be less effective during stress, when tremors are often at their worst. Helmich and his team wanted to investigate whether a medication targeting the stress system could help and how this effect of stress on tremors works in the brain. The work is published in the journal Annals of Neurology.