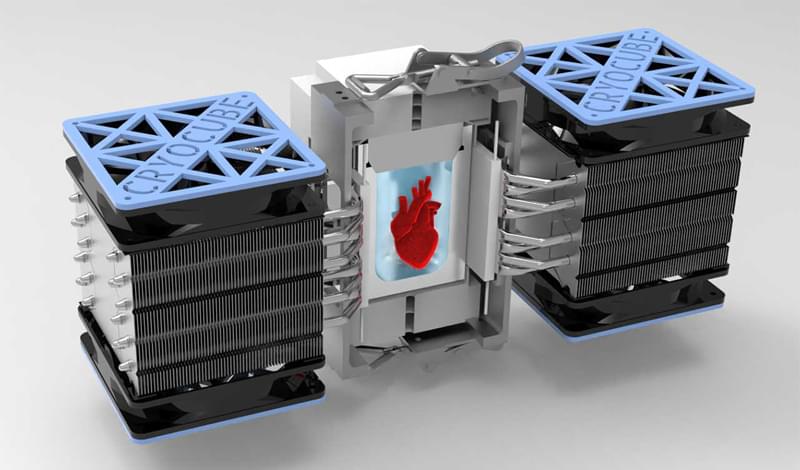
Researchers at the University of California, Berkeley, have successfully revived human heart tissue after it had been preserved in a subfreezing, supercooled state for up to three days.
I’m confused. At 34:20 he says he says people in clinical trials had there age reversed 2 years (I assume he is talking about thymus rejuvenation) and it is additive so people who had it 4 times went back 8 years. Ok. AND?! I mean am I missing something here? Is this not what we are after? I’m 50 now, so if I did it 13 times will I be 24 again?
My guest today is a revolutionary thinker and ground-breaking scientist who’s on a mission to make you younger. He’s Australian biologist and Harvard professor David Sinclair, author of Lifespan: Why We Age – And Why We Don’t Have To. David is one of the world’s leading scientific authorities on longevity, ageing and how to slow its effects.
#feelbetterlivemore.
–
Connect with David:
Instagram https://www.instagram.com/davidsinclairphd.
Facebook https://www.facebook.com/davidsinclairphd/
Twitter https://twitter.com/davidasinclair.
Website https://www.doctorsinclair.com.
About David https://sinclair.hms.harvard.edu/people/david-sinclair.
David’s book:
Lizards can regrow severed tails, making them the closest relative to humans that can regenerate a lost appendage. But in lieu of the original tail that includes a spinal column and nerves, the replacement structure is an imperfect cartilage tube. Now, for the first time, a USC-led study in Nature Communications describes how stem cells can help lizards regenerate better tails.
“This is one of the only cases where the regeneration of an appendage has been significantly improved through stem cell-based therapy in any reptile, bird or mammal, and it informs efforts to improve wound healing in humans,” said the study’s corresponding author Thomas Lozito, an assistant professor of orthopaedic surgery and stem cell biology and regenerative medicine at the Keck School of Medicine of USC.
Talking about RejuvenateBio starts at 20:30. Mentions there are 300 known genes concerning human aging and 45 of those have been tested in mice with what sounds like success.
Wow! Where do I start. I woke up and seen Dr. George Church on Bloomberg news. They was discussing a new biotech startup company called Rejuvenate Bio. A life extension company that seeks to reverse aging in dogs. Then apply that knowledge to humans. I ask Dr. Church about what he thinks is the cause of aging. t. Dr. Church thinks its a genetic reason why we age. Dr. Church is a cofounder of a company called Colossal is a company that wants to create a hybrid between the east asian elephant and the woolly mammoth. The purpose of doing this is to fight climate change and prevent the extinction of the east asian elephant.
As technology rapidly progresses, some proponents of artificial intelligence believe that it will help solve complex social challenges and offer immortality via virtual humans.
But AI’s critics are sounding the alarm, going so far as to call its development an “existential threat” to mankind. Is this the stuff of science fiction? Could the “Terminator” become reality, or will these fears prevent the next technological revolution?
Subscribe for more videos like this: http://bit.ly/1GpwawV
Facebook: http://facebook.com/92ndStreetY
Twitter: https://twitter.com/92Y
Tumblr: http://92y.tumblr.com/
Instagram: http://Instagram.com/92ndStreetY
Vine: https://vine.co/92Y
On Demand: http://www.92yondemand.org
Ray Kurzweil — Singularitarian Immortalist, Director of Engineering at Google, famous inventor, author of How to Create a Mind http://GF2045.com/speakers/.
A world-class prolific inventor and leading futurist author, “the restless genius” (Wall Street Journal) points to 2045 for the technological singularity when A.I. will surpass human intelligence in his New York Times best seller The Singularity is Near, Amazon’s #1 book in science and philosophy.
In this video Ray Kurzweil discusses his predictions about radical life extension, singularity, life expansion and the imminence of physical immortality. He invites participants to the second international Global Future 2045 congress (June 2013) http://www.GF2045.com.
“If we have radical life extension only, we would get profoundly bored, we’d have profound existential ennui, running out of things to do, and new ideas, but that’s not what’s going to happen. In addition to radical life extension, we’re going to have radical life expansion, we’re going to have millions of virtual environments to explore, we’re going to literally expand our brains.”
“We’ll be routinely able to change our bodies very quickly, as well as our environments in virtual reality, but it will feel very real. We’ll ultimately be able to do that with real reality too, like self-organizing swarms of nanobots that can link themselves up into a virtual body.” says Ray Kurzweil.
For more information about the GF2045 congress, please visit http://www.GF2045.com
He says here that we will not live to 150 without merging with technology. Since rejuvenation already exists for worms, mice, and rats I see no reason why a person could not make it that long and longer.
In this video Sergey talks about his ideas for when we will reach Longevity Escape Velocity, his vision for the longer term and the implications for society as people live longer.
Sergey Young is a longevity investor and visionary on a mission to help one billion people extend their lifespans and live longer, healthier lives. To do that, Sergey founded Longevity Vision Fund to accelerate breakthroughs in life extension technology and to make longevity affordable and accessible to all.
Sergey is on the Board of Directors for the American Federation of Aging Research (AFAR) and is the Development Sponsor for AGE REVERSAL XPRIZE’s global competition designed to cure aging.
Sergey Young has been featured as a top longevity expert and contributor on CNN, BBC, Fox News, and Forbes. As the author of books such as ‘The Science and Technology of Growing Young’ and the mastermind behind the online life extension platform SergeyYoung.com, Sergey is passionate about sharing news from the exciting world of longevity.
Researchers have identified a subpopulation of mesenchymal stem cells (MSCs) that boost the healing of bone fractures and show an ability to differentiate into various cell types.
Their findings are published in the journal Bone Reports in a paper titled, “Bone marrow CD73+ mesenchymal stem cells display increased stemness in vitro and promote fracture healing in vivo,” and led by researchers from the University of Tsukuba, in collaboration with the University of Bonn, Germany.
“MSCs are multipotent and considered to be of great potential for regenerative medicine,” the researchers wrote. “We could show recently (Breitbach, Kimura, et al. 2018) that a subpopulation of MSCs, as well as sinusoidal endothelial cells (sECs) in the bone marrow (BM) of CD73-EGFP reporter mice, could be labeled in vivo. We took advantage of this model to explore the plasticity and osteogenic potential of CD73-EGFP+ MSCs in vitro and their role in the regenerative response upon bone lesion in vivo.”

Acclaimed Harvard professor and entrepreneur Dr. David Sinclair believes that we will see human life expectancy increase to at least 100 years within this century. A world in which humans live significantly longer will have a major impact on economies, policies, healthcare, education, ethics, and more. Sinclair joined Bridgewater Portfolio Strategist Atul Lele to discuss the science and societal, political, systemic and ethical implications of humans living significantly longer lives.
Recorded: Aug 30 2021
The Science of Slowing Aging and Increasing Life Expectancy.
0:00 – 19:20
What Increasing Life Expectancy Means for Individuals.
19:20 – 30:40
The Impact on Pension, Healthcare and Education Systems.
30:40 – 44:18
The Economic Benefits of Longer Life Expectancy.