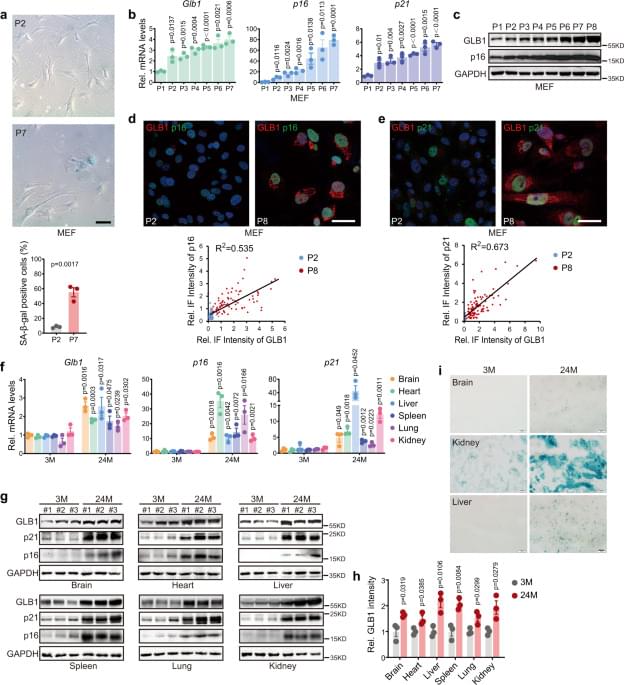
Aging inevitably increases the risk of disease, as exemplified by CAD, AD, and cancer. Monitoring the aging process and understanding its mechanisms will not only enhance early diagnoses, it may also provide strategies for the early prevention and treatment of diseases. While biomarkers for cellular senescence in in vitro cultured mammalian cells are already well-defined, those that define in vivo senescence/aging at the systemic level remain scarce. Here, we generated a targeted Glb1+/m allele at the Glb1 locus that encodes β-galactosidase. The GAC signal indicates Glb1 level. The results reveal that the live-imaged GAC signal is linearly correlated with chronological age, but only in middle-aged mice (9–13 months). High GAC at the MA stage was associated with cardiac hypertrophy and shortened lifespan. Moreover, GAC signal was exponentially increased in pathological lung fibrosis induced by BLM. Thus, this in vivo reporter mouse can faithfully monitor systemic aging and organ functional decline in a manner closely associated with lifespan, and provides an ideal system for studying aging mechanisms and developing anti-aging manipulations.
The upregulation of p16Ink4a transcription and elevated SAβ-gal staining are both well-established and widely used biomarkers for cellular senescence17, and the former led to the generation of live-imaging aging reporter mice20,22,23. Intriguingly, high level of p16Ink4a, indicated by luciferase activity, predicts cancer initiation rather than lifespan. Similarly, the in vivo application of SAβ-gal as a senescence marker at the tissue level is also limited. Positive SAβ-gal-staining is easy to obtain in kidney and adipose tissue sections but difficult to obtain in blood vessel and heart sections. By SAβ-gal staining, not many positive cells were detected in old individuals26. It raises the question of whether SAβ-gal labels in vivo senescence or if the percentage of in vivo senescent cells is indeed very low.