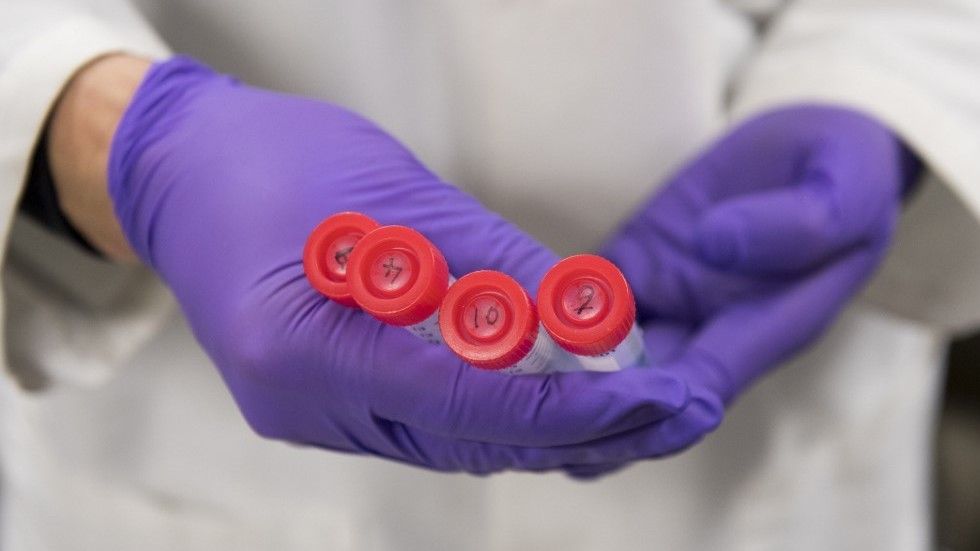
A new study by researchers from the Dexeus Women’s Health research network in Barcelona found that frozen sperm samples survived when exposed to microgravity.
That could mean that sperm banks in space are possible, providing future space travelers with the ability to reproduce in space with sperm samples brought up from Earth.
“Some studies suggest a significant decrease in the motility of a human, fresh sperm sample,” Montserrat Boada who presented the research yesterday at an annual meeting in Vienna, Austria, said, as quoted by The Guardian. “But nothing has been reported on the possible effects of gravitational differences on frozen human gametes, in which state they could be transported from Earth to space.”