Dr. Arye Elfenbein, MD, PhD, is the Co-Founder of Wildtype (https://www.wildtypefoods.com/), a biotechnology company which produces cultured seafood (with a focus on cultivated Pacific salmon) from fish cells, sustainably and cost effectively, with the nutritional benefits, but without common contaminants such as mercury, microplastics, antibiotics, or pesticides, and without relying on commercial fishing or fish farming.
Born in Israel and raised in Australia, Dr. Elfenbein combines his deep passion for medicine and unique childhood connection to the ocean to fuel Wildtype’s health and environmental mission.
After studying at Dartmouth and Kyoto University, attaining a PhD and MD, Dr. Elfenbein began his residency at Yale where he first trained in Internal Medicine before completing training in Cardiology. After residency, he moved to San Francisco to work with Professor Dr. Deepak Srivastava at the revered Gladstone Institutes / UCSF, also known for being the scientific homes of Nobel laureates Dr. Shinya Yamanaka (iPs cells) and Dr. Jennifer Doudna (CRISPR).
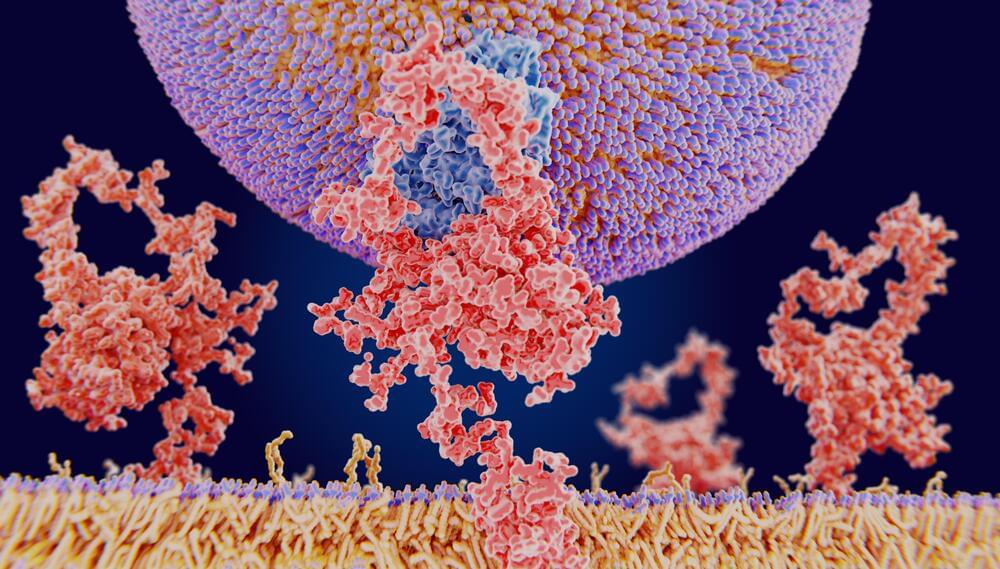
During his time at the Gladstone Institutes, Dr. Elfenbein’s research focused on cardiac regeneration following heart attacks. This research inspired him to apply the principles of stem cell biology beyond medicine, and to address the growing problems in our food system.
When away from Wildtype, Dr. Elfenbein continues to work as a cardiologist with a focus on critical care, lending his expertise and passion for patient care to the ICU.