Cheers!
𝐁𝐞𝐞𝐫 𝐈𝐧𝐠𝐫𝐞𝐝𝐢𝐞𝐧𝐭 𝐌𝐚𝐲 𝐈𝐧𝐡𝐢𝐛𝐢𝐭 𝐂𝐥𝐮𝐦𝐩𝐢𝐧𝐠 𝐨𝐟 𝐀𝐥𝐳𝐡𝐞𝐢𝐦𝐞𝐫’𝐬 𝐏𝐫𝐨𝐭𝐞𝐢𝐧
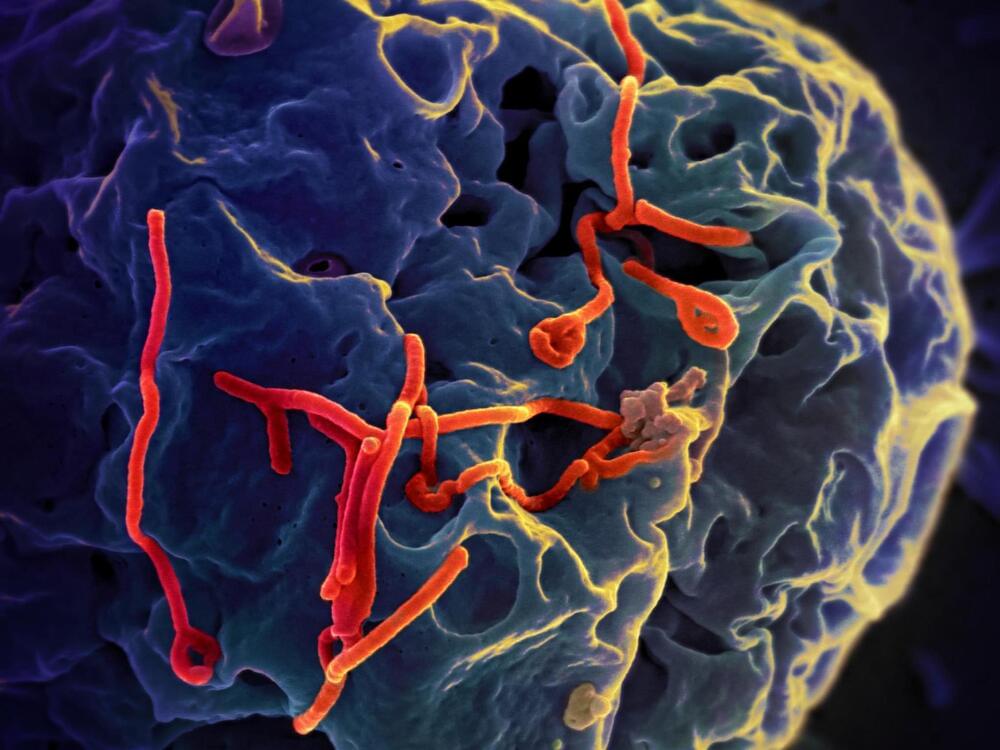
𝘽𝙚𝙚𝙧 𝙞𝙨 𝙤𝙣𝙚 𝙤𝙛 𝙩𝙝𝙚 𝙤𝙡𝙙𝙚𝙨𝙩 𝙖𝙣𝙙 𝙢𝙤𝙨𝙩 𝙥𝙤𝙥𝙪𝙡𝙖𝙧 𝙗𝙚𝙫𝙚𝙧𝙖𝙜𝙚𝙨 𝙞𝙣 𝙩𝙝𝙚 𝙬𝙤𝙧𝙡𝙙, 𝙬𝙞𝙩𝙝 𝙨𝙤𝙢𝙚 𝙥𝙚𝙤𝙥𝙡𝙚 𝙡𝙤𝙫𝙞𝙣𝙜 𝙖𝙣𝙙 𝙤𝙩𝙝𝙚𝙧𝙨 𝙝𝙖𝙩𝙞𝙣𝙜 𝙩𝙝𝙚 𝙙𝙞𝙨𝙩𝙞𝙣𝙘𝙩, 𝙗𝙞𝙩𝙩𝙚𝙧 𝙩𝙖𝙨𝙩𝙚 𝙤𝙛 𝙩𝙝𝙚 𝙝𝙤𝙥𝙨 𝙪𝙨𝙚𝙙 𝙩𝙤 𝙛𝙡𝙖𝙫𝙤𝙧 𝙞𝙩𝙨 𝙢𝙖𝙣𝙮 𝙫𝙖𝙧𝙞𝙚𝙩𝙞𝙚𝙨. 𝘽𝙪𝙩 𝙖𝙣 𝙚𝙨𝙥𝙚𝙘𝙞𝙖𝙡𝙡𝙮 “𝙝𝙤𝙥𝙥𝙮” 𝙗𝙧𝙚𝙬 𝙢𝙞𝙜𝙝𝙩 𝙝𝙖𝙫𝙚 𝙪𝙣𝙞𝙦𝙪𝙚 𝙝𝙚𝙖𝙡𝙩𝙝 𝙗𝙚𝙣𝙚𝙛𝙞𝙩𝙨. 𝙍𝙚𝙘𝙚𝙣𝙩 𝙧𝙚𝙨𝙚𝙖𝙧𝙘𝙝 𝙥𝙪𝙗𝙡𝙞𝙨𝙝𝙚𝙙 𝙞𝙣 𝘼𝘾𝙎 𝘾𝙝𝙚𝙢𝙞𝙘𝙖𝙡 𝙉𝙚𝙪𝙧𝙤𝙨𝙘𝙞𝙚𝙣𝙘𝙚 𝙧𝙚𝙥𝙤𝙧𝙩𝙨 𝙩𝙝𝙖𝙩 𝙘𝙝𝙚𝙢𝙞𝙘𝙖𝙡𝙨 𝙚𝙭𝙩𝙧𝙖𝙘𝙩𝙚𝙙 𝙛𝙧𝙤𝙢 𝙝𝙤𝙥 𝙛𝙡𝙤𝙬𝙚𝙧𝙨 𝙘𝙖𝙣, 𝙞𝙣 𝙡𝙖𝙗 𝙙𝙞𝙨𝙝𝙚𝙨, 𝙞𝙣𝙝𝙞𝙗𝙞𝙩 𝙩𝙝𝙚 𝙘𝙡𝙪𝙢𝙥𝙞𝙣𝙜 𝙤𝙛 𝙖𝙢𝙮𝙡𝙤𝙞𝙙 𝙗𝙚𝙩𝙖 𝙥𝙧𝙤𝙩𝙚𝙞𝙣𝙨, 𝙬𝙝𝙞𝙘𝙝 𝙞𝙨 𝙖𝙨𝙨𝙤𝙘𝙞𝙖𝙩𝙚𝙙 𝙬𝙞𝙩𝙝 𝘼𝙡𝙯𝙝𝙚𝙞𝙢𝙚𝙧’𝙨 𝙙𝙞𝙨𝙚𝙖𝙨𝙚 (𝘼𝘿).
Beer is one of the oldest and most popular beverages in the world, with some people loving and others hating the distinct, bitter taste of the hops used to flavor its many varieties. But an especially “hoppy” brew might have unique health benefits. Recent research published in ACS Chemical Neuroscience reports that chemicals extracted from hop flowers can, in lab dishes, inhibit the clumping of amyloid beta proteins, which is associated with Alzheimer’s disease (AD).
AD is a debilitating neurodegenerative disease, often marked by memory loss and personality changes in older adults. Part of the difficulty in treating the disease is the time lag between the start of underlying biochemical processes and the onset of symptoms, with several years separating them. This means that irreversible damage to the nervous system occurs before one even realizes they may have the disease. Accordingly, preventative strategies and therapeutics that can intervene before symptoms appear are of increasing interest.
One of these strategies involves “nutraceuticals,” or foods that have some type of medicinal or nutritional function. The hop flowers used to flavor beers have been explored as one of these potential nutraceuticals, with previous studies suggesting that the plant could interfere with the accumulation of amyloid beta proteins associated with AD. So, Cristina Airoldi, Alessandro Palmioli and colleagues wanted to investigate which chemical compounds in hops had this effect.