There should be some vaccine against common cold because globally millions of people suffer s due to this disease.
Vaccines are an effective public health strategy, but so far, science has not been able to develop one for the common cold.

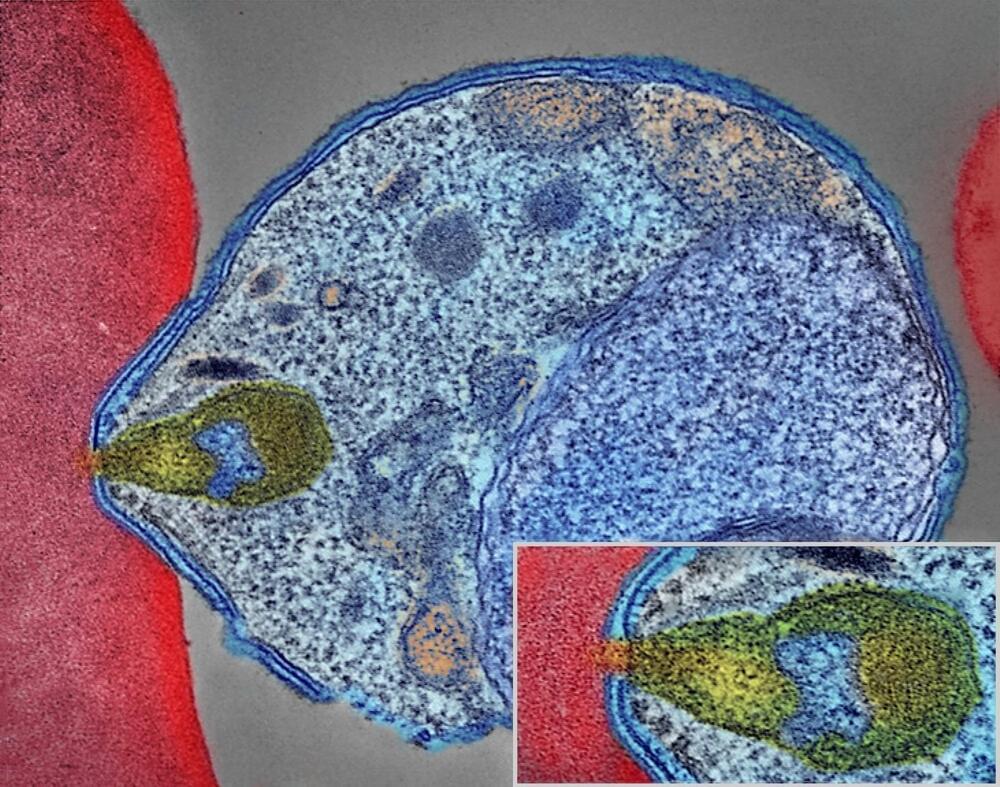
In a recent study published in Scientific Reports, researchers identified serological Hepatitis C virus (HCV) signatures and human immunodeficiency virus (HIV) signatures through the secondary utilization of ribonucleic acid sequencing (RNA-seq) analysis data among previous and existing smokers with or without COPD (chronic obstructive pulmonary disease).
Viral detection by RNA sequencing analysis has increased the knowledge base of viruses causing human infections. Identifying undiagnosed viral infections by using existing nucleic acid sequencing data could facilitate epidemiological survey-based analysis and aid in the development of diagnostic and therapeutic options for improved population health.

If you enjoy some good toilet technology, then I think “urine” for a treat. Starling Medical is poised to launch its at-home urine diagnostic patient-monitoring platform, dubbed “StarStream,” that doesn’t rely on the traditional catching containers or dipsticks.
Now, if you’re thinking this technology sounds familiar, you would be correct: My colleague Haje Jan Kamps wrote about Withings’ U-Scan, a urinalysis device, earlier this month when the health-focused consumer tech company debuted it at CES. U-Scan also sits in the toilet for at-home monitoring.
However, Alex Arevalos, Starling’s co-founder and CEO, told TechCrunch that this is an underserved market — the global urinalysis market is forecasted to be valued at $4.9 billion by 2026, meaning there is plenty of room for Withings and a scrappy startup.
On Nov. 26, 2022 a SpaceX Falcon 9 rocket departed from departed from NASA’s Kennedy Space Center in Florida to deliver supplies to the International Space Station. Among the 7,700 pounds of cargo on board, it is safe to say that the smallest delivery that day were a bunch of frozen bacteria.
In an interdisciplinary collaboration, a group of scientists from MIT Media Lab, NREL, Seed Health and others, bioengineered a plastic-eating bacteria to be able to upcycle plastics. Mashable met with some of them to find out how the bacteria works, why it was it was sent to space, and how it can help humanity tackle plastic pollution in space as well as on Earth.
Mashable is your source for the latest in tech, culture, and entertainment.
Follow us:
Check out https://mashable.com/
Facebook: https://www.facebook.com/mashable.
Twitter: https://twitter.com/mashable.
Instagram: https://www.instagram.com/mashable
A monoclonal antibody treatment was found to be safe, well tolerated, and effective in protecting against malaria in a small group of healthy volunteers who were exposed to malaria in a challenge study, according to new research published in The Lancet Infectious Diseases by researchers at the University of Maryland School of Medicine (UMSOM).
“The study demonstrates the feasibility of using monoclonal antibody therapies to help prevent malarial infection and holds promise for deployment to places where the disease is endemic,” said Kirsten Lyke, MD, Professor of Medicine and Director of the Malaria Vaccine and Challenge Unit in the Center for Vaccine Development and Global Health (CVD) at UMSOM. “This may allow us to revisit malaria eradication efforts.”
There were 241 million malaria cases and 627,000 deaths reported worldwide in 2020 alone, which is a 12 percent increase from 2019. Public health experts contend new strategies are urgently needed to achieve the United Nation’s sustainable development goal of 90 percent reduction in malaria incidence and mortality by 2030. Scientists have tried for decades to develop a highly effective malaria vaccine without much success.

A novel virus, potentially fatal to whales and dolphins, has been discovered by researchers at the University of Hawaiʻi Health and Stranding Lab. Prior to its discovery in 10 whale and dolphin host species across the Pacific, the virus was found in only a single marine mammal worldwide, a Longman’s beaked whale stranded on Maui in 2010. The findings are published in Frontiers in Marine Science.
The discovery of beaked whale circovirus (BWCV) in whales and dolphins expands the knowledge of marine mammal species that can become infected with the disease. Circoviruses are DNA viruses that cause disease in birds, pigs and dogs, and in severe cases can become fatal.
“Our study found Cuvier’s beaked whales tested positive for BWCV in Saipan and American Samoa, nearly 4,000 miles away from the first discovered case,” said Kristi West, director of the UH Health and Stranding Lab. “The positive cases found outside of Hawaiʻi were surprising, and indicates that this virus is spread across the Central and Western Pacific and may have a global presence in marine mammals.”

Health care integration has long been touted as a panacea for reining in health care costs and boosting quality of care.
But integrated health systems appear to be failing on both fronts, according to the results of a new nationwide study led by researchers at Harvard and the National Bureau of Economic Research (NBER).
Instead, the analysis finds marginally better care at significantly higher costs for patients seen in health systems, compared to those at independent practices or hospitals.
Researchers at Stanford Medicine have shown they can measure thousands of molecules — some of which are signals of health — from a single drop of blood.
The new approach combines a microsampling device — a tool used to self-administer a finger prick — with “multi-omics” technologies, which simultaneously analyze a vast array of proteins, fats, by-products of metabolism and inflammatory markers.
“Even more importantly, we’ve shown you can collect the blood drop at home and mail it into the lab,” said Michael Snyder, PhD, director of the Center for Genomics and Personalized Medicine and senior author on the research, which was published in Nature Biomedical Engineering on Jan. 19.
Nearly 15,500 people in the U.S. over age 50 are estimated to have VEXAS syndrome.
A rare disorder called VEXAS syndrome has bemused the United States’ health services since 2020. The syndrome was a great mystery until the researchers’ work yielded results.
As stated by NYU Langone Health, with up to 50 percent of sufferers, mostly men, passing away within five years of diagnosis, this illness has a significant mortality rate.
BlackJack3D/iStock.
A new study led by the NYU Grossman School of Medicine has shown that about 13,200 men and another 2,300 women in the United States over age 50 are estimated to have VEXAS syndrome.

More than one-third of UK health experts are not aware of Charles Bonnet syndrome — CBS — a condition which can cause vivid, and sometimes frightening, hallucinations.
A poll of 1,100 health experts — including GPs, doctors and optometrists — found 37 per cent were not aware of CBS.
The condition is not caused by mental health problems or dementia. It is purely due to a loss of sight — 60 per cent or more — which reduces or stops the regular messages from the eye to the brain.