An experimental new vaccine claims to be able to change human DNA and could be deployed against COVID-19 by 2021 through a biochip implant.
The most significant scientific discovery since gravity has been hiding in plain sight for nearly a decade and its destructive potential to humanity is so enormous that the biggest war machine on the planet immediately deployed its vast resources to possess and control it, financing its research and development through agencies like the National Institutes of Health (NIH), the Defense Advanced Research Projects Agency (DARPA) and HHS’ BARDA.
The revolutionary breakthrough came to a Canadian scientist named Derek Rossi in 2010 purely by accident. The now-retired Harvard professor claimed in an interview with the National Post that he found a way to “reprogram” the molecules that carry the genetic instructions for cell development in the human body, not to mention all biological lifeforms.
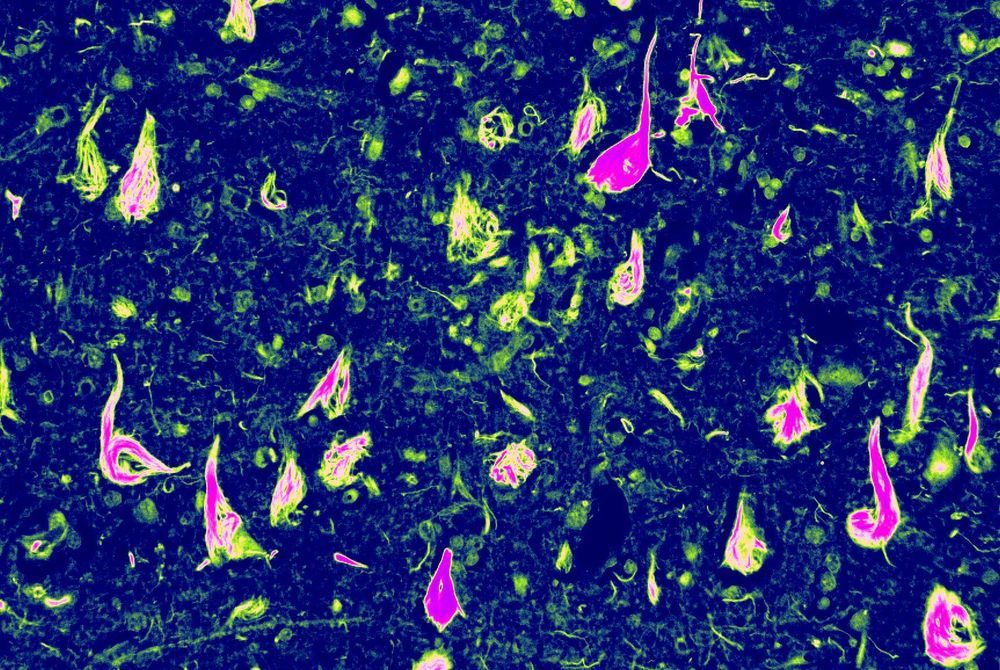
These molecules are called ‘messenger ribonucleic acid’ or mRNA and the newfound ability to rewrite those instructions to produce any kind of cell within a biological organism has radically changed the course of Western medicine and science, even if no one has really noticed yet. As Rossi, himself, puts it: “The real important discovery here was you could now use mRNA, and if you got it into the cells, then you could get the mRNA to express any protein in the cells, and this was the big thing.”