🏥 💻 🚑
Study in Npj Digital Medicine evaluates COMPOSER, a deep learning model for early sepsis prediction, showing its effectiveness in improving patient care and reducing in-hospital mortality rates.

People with unusually thin retinas are at greater risk of later developing bronchitis and other conditions, suggesting retinal scans could eventually become a component of routine health screening.
But then Santamaria, who is at the University of Calgary in Canada, came up with a bold idea. Maybe he could use these particles as a therapy to target and quiet, or even kill, the cells responsible for driving the disease — those that destroy insulin-producing islet cells in the pancreas. It seemed like a far-fetched idea, but he decided to try it. “I kept doing experiment after experiment,” he says. Now, more than two decades later, Santamaria’s therapy is on the cusp of being tested in people.
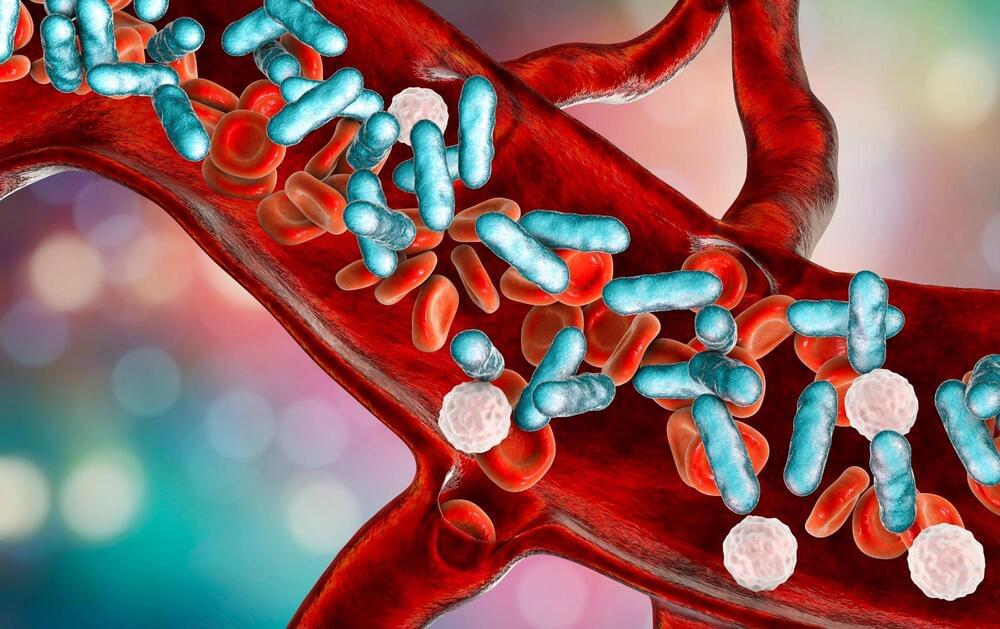
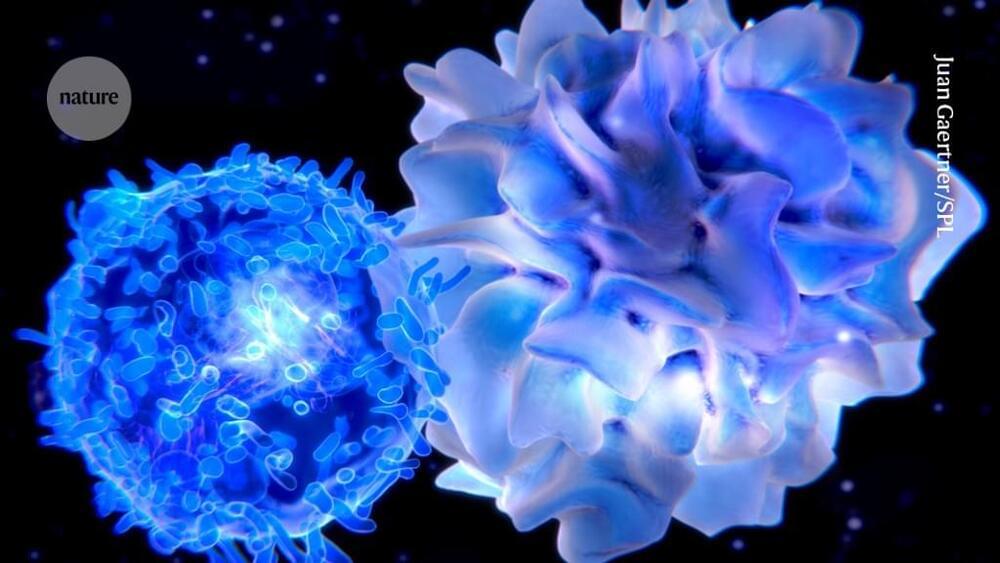
It’s not alone. Researchers have been trying for more than 50 years to tame the cells that are responsible for autoimmune disorders such as type 1 diabetes, lupus and multiple sclerosis. Most of the approved therapies for these conditions work by suppressing the entire immune response. This often alleviates symptoms but leaves people at elevated risk of infections and cancers.
But for decades, immunologists have hoped to restore what’s known as tolerance — the immune system’s ability to ignore antigens that belong in the body while appropriately attacking those that don’t. In some cases, that means administering the very antigens that the rogue cells are trained to attack, a strategy that can deprogram the cells and dampen the autoimmune response. Other researchers are trying to selectively wipe out the problematic cells, or to introduce suppressive immune cells that have been engineered to target them. One approach that relies on engineered immune cells was used to treat 15 people with lupus or other immune disorders with surprising success1. One participant has been symptom-free for more than two and a half years.

I hope more research is fruitful because I got the doctor’s results from my recent colonoscopy. The polyps are benign but pre cancerous. I go back in 5 years and I’ll be eating healthier and exercising. I gotta admit I don’t feel great but it could be something I ate.
Scientists in China have demonstrated a new kind of antidepressant could also have the potential to restore the body’s ability to fight some types of cancer.
In strategic combination with anti-tumor drugs, the oral antidepressant ansofaxine hydrochloride appears to inhibit colon cancer cell growth in cell cultures and in mice, strengthening the immune system and inducing a form of programmed cell death.
Yet to be tested on humans, it’s unclear how the results will translate as an actual cancer treatment.

Researchers at City of Hope and Translational Genomics Research Institute (TGen) have developed and tested an innovative machine-learning approach that could one day enable the earlier detection of cancer in patients by using smaller blood draws. The study is published in the journal Science Translational Medicine.
“A huge body of evidence shows that cancer caught at later stages kills people. This new technology gets us closer to a world where people will receive a blood test annually to detect cancer earlier when it is more treatable and possibly curable,” said Cristian Tomasetti, Ph.D., corresponding author of the new study and director of City of Hope’s Center for Cancer Prevention and Early Detection.
Tomasetti explained that 99% of people diagnosed with Stage 1 breast cancer will be alive five years later; however, if it is found at Stage 4, when disease has spread to other organs, the five-year survival drops to 31%.

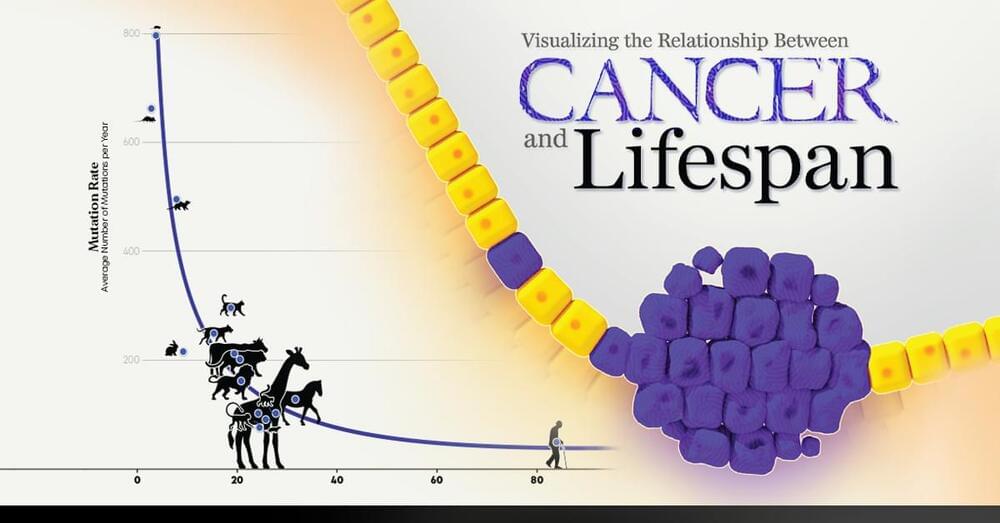
Aging is a common phenomenon among organisms, however, lifespan tends to vary across different species to a significant extent among vertebrates themselves. Aging occurs due to the gradual increase in DNA damage, disruption of cellular organelles, deregulation of protein function, disrupted metabolism and oxidative stress [1].
Longevity. Technology: The differences in lifespan are driven by trade-offs and evolutionary trajectories in the genomes of organisms. Age-specific selection also impacts allele (variations of a gene) frequencies in a population. This in turn impacts environment-specific mortality risk and disease susceptibility. Moreover, mutational processes are influenced by life history and age in both somatic and germline cells.
Now, a new review published in Trends in Genetics discusses recent advances in the evolution of aging at population, organismal and cellular scales.
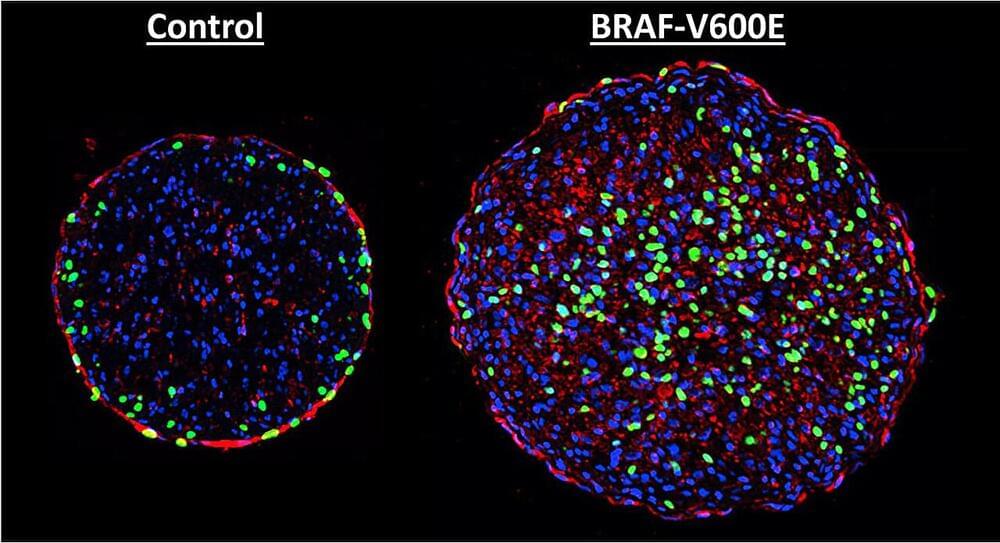
Biomedical engineers at Duke University have demonstrated that one of the most dangerous mutations found in skin cancers might moonlight as a pathway to mending a broken heart.
The genetic mutation in the protein BRAF, a part of the MAPK signaling pathway that can promote cell division, is one of the most common and most aggressive found in melanoma patients. In a new study, researchers show that introducing this mutation to rat heart tissue grown in a laboratory can induce growth.
Repairing cardiac muscle after a heart attack is the “holy grail” of heart research, complicated by the fact that heart tissue does not regenerate on its own. One potential strategy would be to persuade heart muscle cells to divide by safely delivering a therapeutic gene to patients and fully controlling its activity in the heart.
