Carbon nanotubes are one of the most elastically strong materials out there.
When I was a kid, I used to take allowance money and occasionally buy rubber-band-powered balsa wood airplanes at a local store. Maybe you’ve seen these. You wind up the rubber band, which stretches the elastomer and stores energy in the elastic strain of the polymer, as in Hooke’s Law (though I suspect the rubber band goes well beyond the linear regime when it’s really wound up, because of the higher order twisting that happens). Rhett Alain wrote about how well you can store energy like this. It turns out that the stored energy per mass of the rubber band can get pretty substantial.
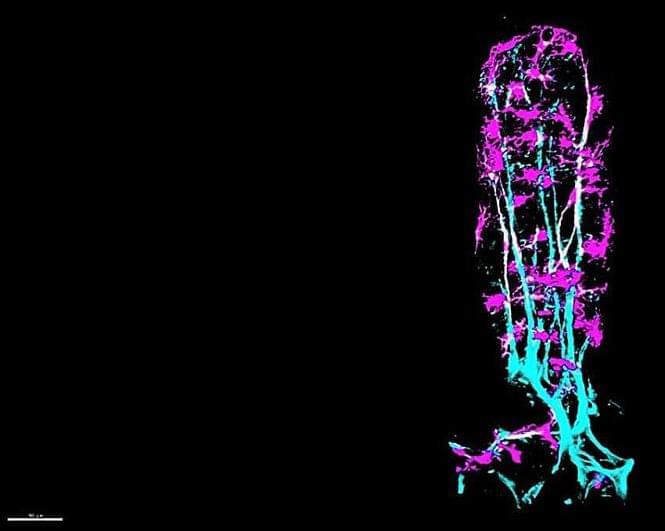
Carbon nanotubes are one of the most elastically strong materials out there. A bit over a decade ago, a group at Michigan State did a serious theoretical analysis of how much energy you could store in a twisted yarn made from single-walled carbon nanotubes. They found that the specific energy storage could get as large as several MJ/kg, as much as four times what you get with lithium ion batteries!
Now, a group in Japan has actually put this to the test, in this Nature Nano paper. They get up to 2.1 MJ/kg, over the lithium ion battery mark, and the specific power (when they release the energy) at about \(10^{6}\) W/kg is not too far away from non-cyclable energy storage media, like TNT. Very cool!