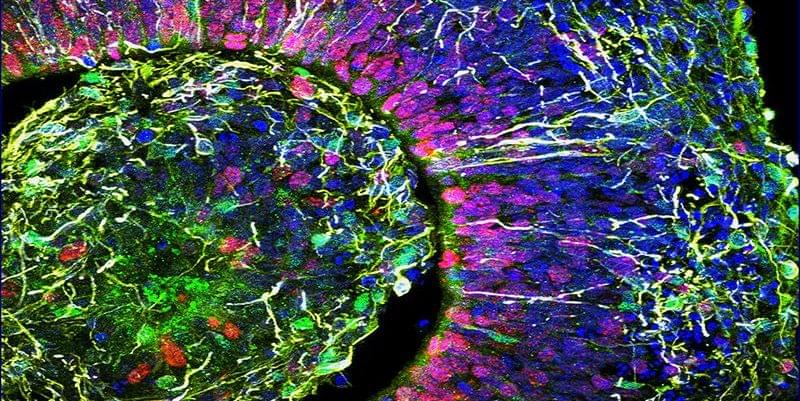
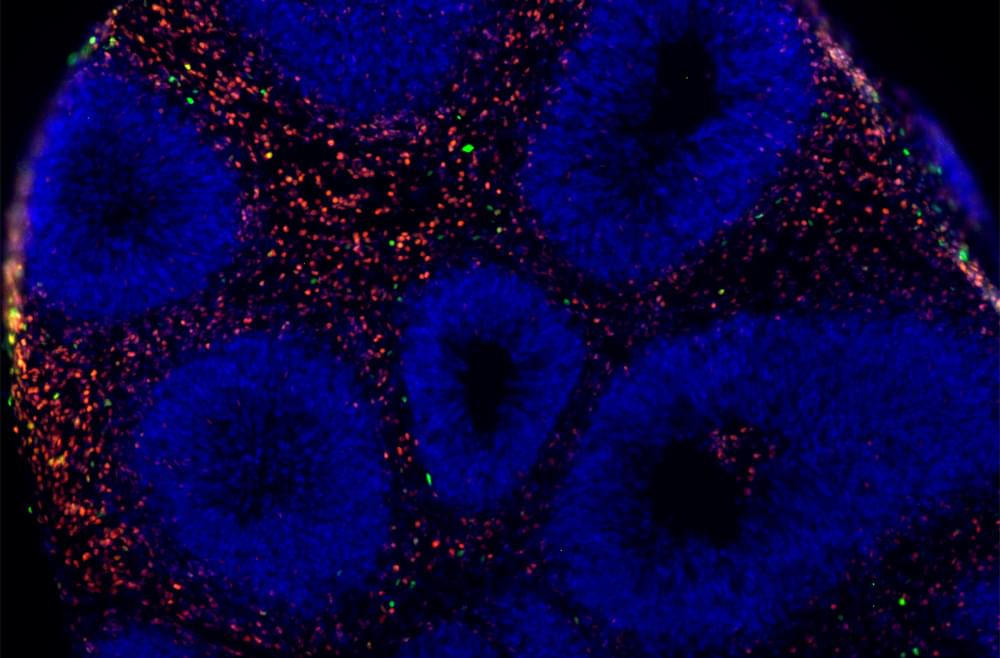
Neurosurgeons can leave the operating room more confident today than ever before about their patient’s brain tumor diagnosis, thanks to the integration of a new system that employs optical imaging and artificial intelligence that are making brain tumor diagnosis quicker and more accurate. This technology is allowing them to quickly see diagnostic tissue and tumor margins in near-real time.
For the full story, visit: http://michmed.org/gk8ZD
Learn more about the scientific breakthroughs happening at Michigan Medicine, visit: https://labblog.uofmhealth.org/
Follow Michigan Medicine on Social:
Twitter: https://twitter.com/umichmedicine.
Instagram: https://www.instagram.com/umichmedicine/
Facebook: https://www.facebook.com/MichiganMedicine/