Cancer is a malignant disease referring to the uncontrollable proliferation of mutated cells. Millions of individuals are affected by cancer each year in the United States alone. Unfortunately, treatment is limited due to the heterogeneity of the disease and different components, which drive the disease to progress. The proliferation of cells can occur anywhere in the body including different organs such as breast, lung, pancreas, and head and neck. Cancer can also affect the reproductive tract in both men and women including the testes and ovaries, respectively. Particularly, ovarian cancer is linked with breast cancer and can result in infertility due to late detection. Due to limited therapeutic efficacy in ovarian cancer, more research is necessary for a meaningful solution. Different groups are working to more effectively target ovarian cancer through different biologic approaches.
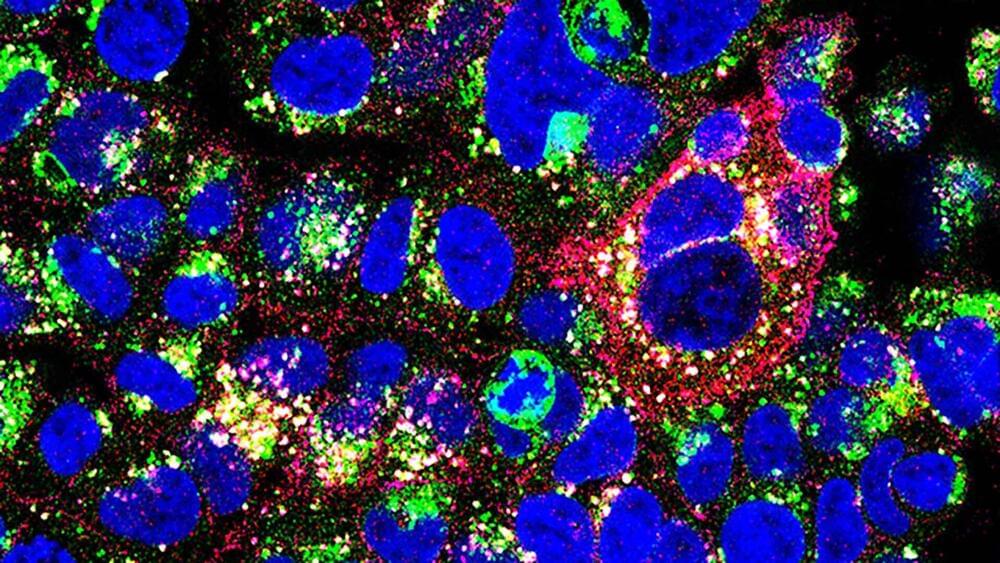
Dr. David B. Weiner and his team from the Wistar Institute recently published an article in Science Advances demonstrating enhanced immunotherapeutic effects in ovarian cancer patients. Immunotherapy refers to a form of cancer therapy that directs the immune system to attack the tumor. In many immunotherapies, immune cells, such as T cells, are activated to kill tumors. This is a unique approach to target cancer compared to chemotherapy or radiation, which tries to directly kill tumor cells and elicit an immune response. Immunotherapy allows the immune system to recognize the tumor and react through the body’s immune system. One prominent immune cell includes natural killer (NK) cells which responsible for initial lying or killing of foreign particles. Novel work has tried to engineer NK cells to target tumors by recognizing unique receptors on its surface.
Weiner’s team and collaborator, Mohamed Abdel-Mohsen, have engineered monoclonal antibodies to engage NK cells to lyse cancer. Interestingly, the team demonstrated this immunotherapeutic regimen optimized preclinical output in mice when combined with checkpoint inhibitors, another type of immunotherapy. The group engineered antibodies to target a glyco-immune marker on most NK cells referred to as Sialic acid-binding immunoglobulin-type lectin (Siglec-7). The novel combination strategy targets NK cells through Siglec-7 and T cells to optimize immune response against tumor cells. The monoclonal antibody (mAb) targeting Siglec-7 allows NK cells to become activated and kill ovarian cancer cells without killing non-cancer cells, which improve specificity and reduce toxicity for patients. Consequently, this antibody resulted in generating a new class of NK cell engagers (NKCE).