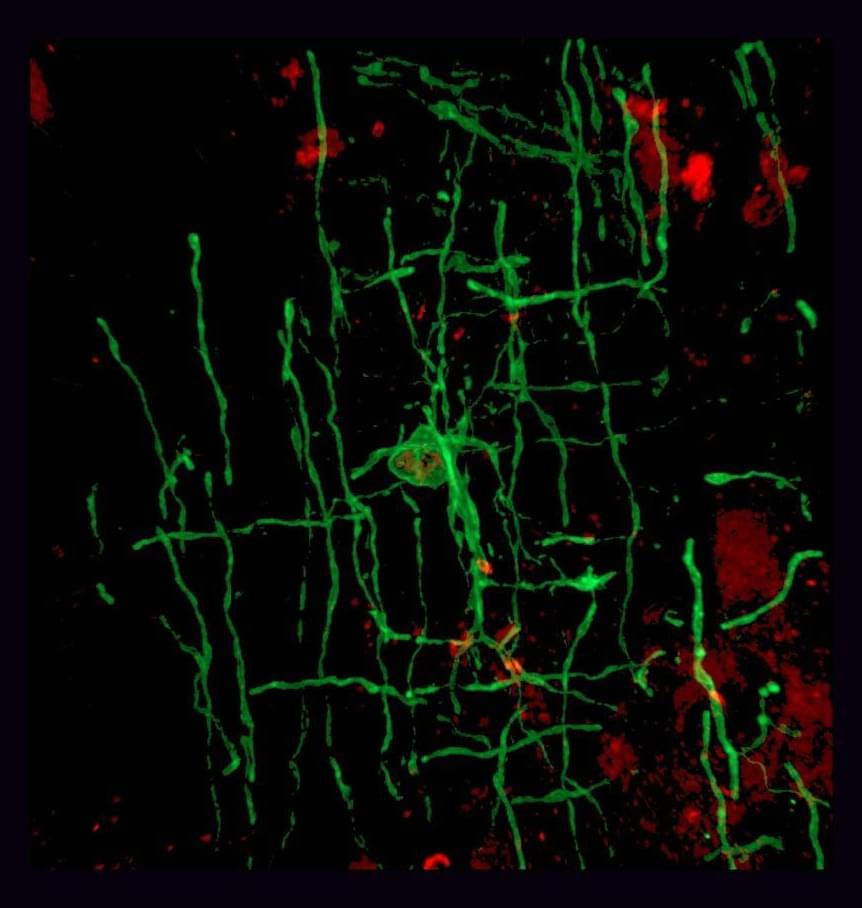
Researchers report in the journal Cell that ancient viruses may be to thank for myelin—and, by extension, our large, complex brains.
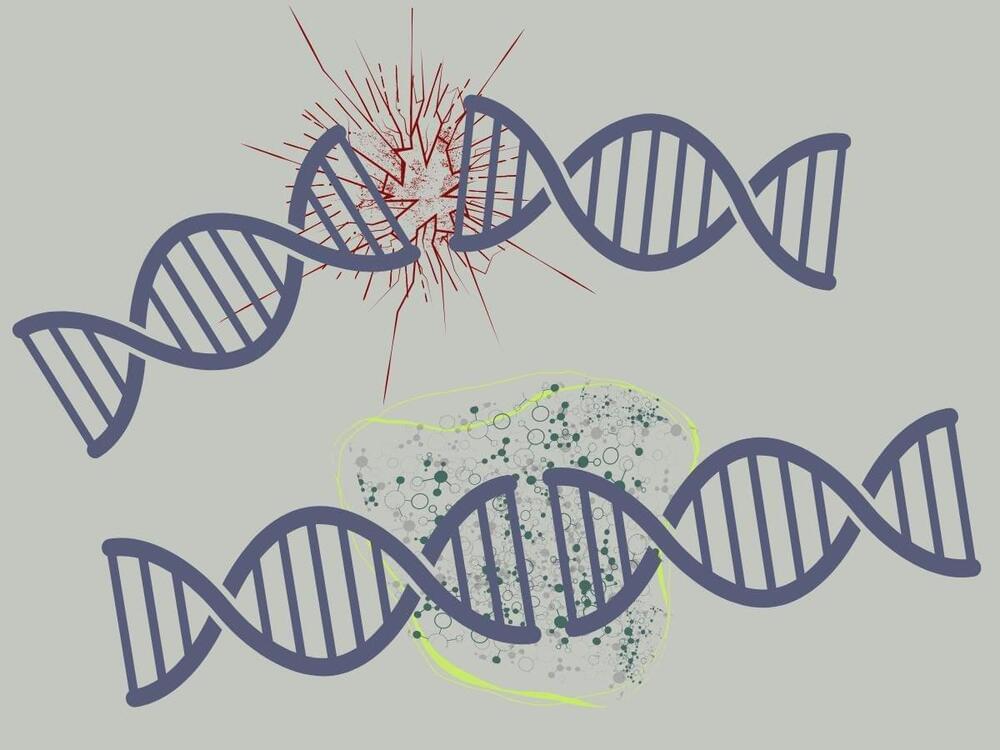
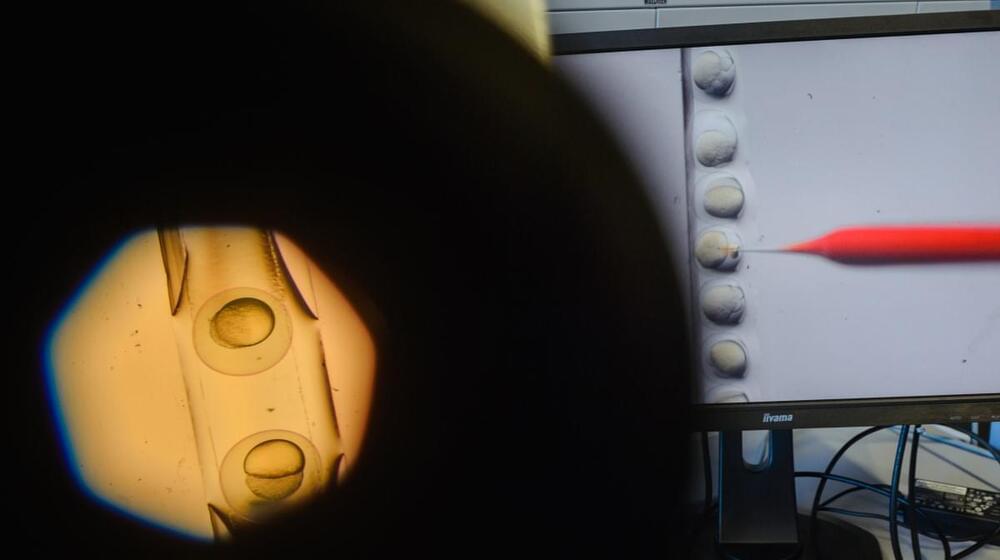
The team found that a retrovirus-derived genetic element or “retrotransposon” is essential for myelin production in mammals, amphibians, and fish. The gene sequence, which they dubbed “RetroMyelin,” is likely a result of ancient viral infection, and comparisons of RetroMyelin in mammals, amphibians, and fish suggest that retroviral infection and genome-invasion events occurred separately in each of these groups.
“Retroviruses were required for vertebrate evolution to take off,” says senior author and neuroscientist Robin Franklin of Altos Labs-Cambridge Institute of Science. “If we didn’t have retroviruses sticking their sequences into the vertebrate genome, then myelination wouldn’t have happened, and without myelination, the whole diversity of vertebrates as we know it would never have happened.”