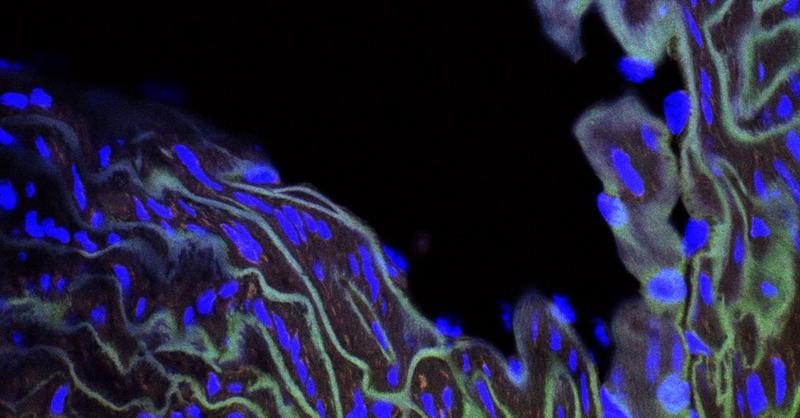
A recent study from the University of California San Diego School of Medicine, investigating meditation as a treatment for chronic lower back pain, has revealed that men and women use different biological mechanisms for pain relief. Men primarily rely on the release of endogenous opioids, the body’s natural painkillers, whereas women depend on alternative, non-opioid pathways to manage pain.
Synthetic opioid drugs, such as morphine and fentanyl, are the most powerful class of painkilling drugs available. Women are known to respond poorly to opioid therapies, which use synthetic opioid molecules to bind to the same receptors as naturally occurring endogenous opioids. This aspect of opioid drugs helps explain why they are so powerful as painkillers, but also why they carry a significant risk of dependence and addiction.
“Dependence develops because people start taking more opioids when their original dosage stops working,” said Fadel Zeidan, Ph.D., professor of anesthesiology and Endowed Professor in Empathy and Compassion Research at UC San Diego Sanford Institute for Empathy and Compassion. “Although speculative, our findings suggest that maybe one reason that females are more likely to become addicted to opioids is that they’re biologically less responsive to them and need to take more to experience any pain relief.”