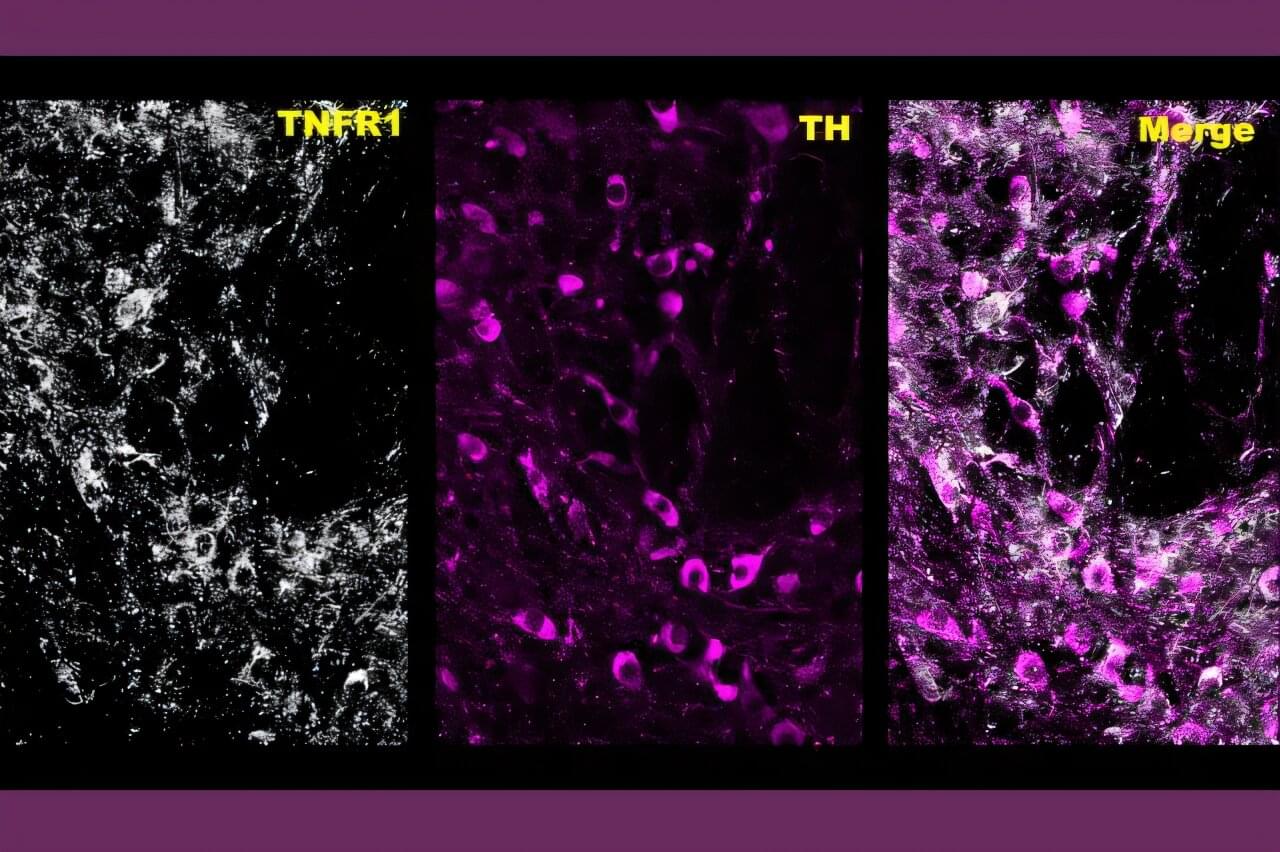
Artificial intelligence (AI) is increasingly used to analyze medical images, materials data and scientific measurements, but many systems struggle when real-world data do not match ideal conditions. Measurements collected from different instruments, experiments or simulations often vary widely in resolution, noise and reliability. Traditional machine-learning models typically assume those differences are negligible—an assumption that can limit accuracy and trustworthiness.
To address this issue, Penn State researchers have developed a new artificial intelligence framework with potential implications for fields ranging from Alzheimer’s disease research to advanced materials design. The approach, called ZENN and detailed in a study that was featured as a showcase in the Proceedings of the National Academy of Sciences, teaches AI models to recognize and adapt to hidden differences in data quality rather than ignoring them.
ZENN, short for Zentropy-Embedded Neural Networks, was developed by Shun Wang, postdoctoral scholar of materials science and engineering; Wenrui Hao, professor of mathematics, Zi-Kui Liu, professor of materials science and engineering, and Shunli Shang, research professor of materials science and engineering.