Scientists have outlined exactly how embryonic stem cells protect other cells from the effects of oxidative stress, thus preventing cellular aging.
Detecting cancer in the earliest stages could dramatically reduce cancer deaths because cancers are usually easier to treat when caught early. To help achieve that goal, MIT and Microsoft researchers are using artificial intelligence to design molecular sensors for early detection.
The researchers developed an AI model to design peptides (short proteins) that are targeted by enzymes called proteases, which are overactive in cancer cells. Nanoparticles coated with these peptides can act as sensors that give off a signal if cancer-linked proteases are present anywhere in the body.
Depending on which proteases are detected, doctors would be able to diagnose the particular type of cancer that is present. These signals could be detected using a simple urine test that could even be done at home.
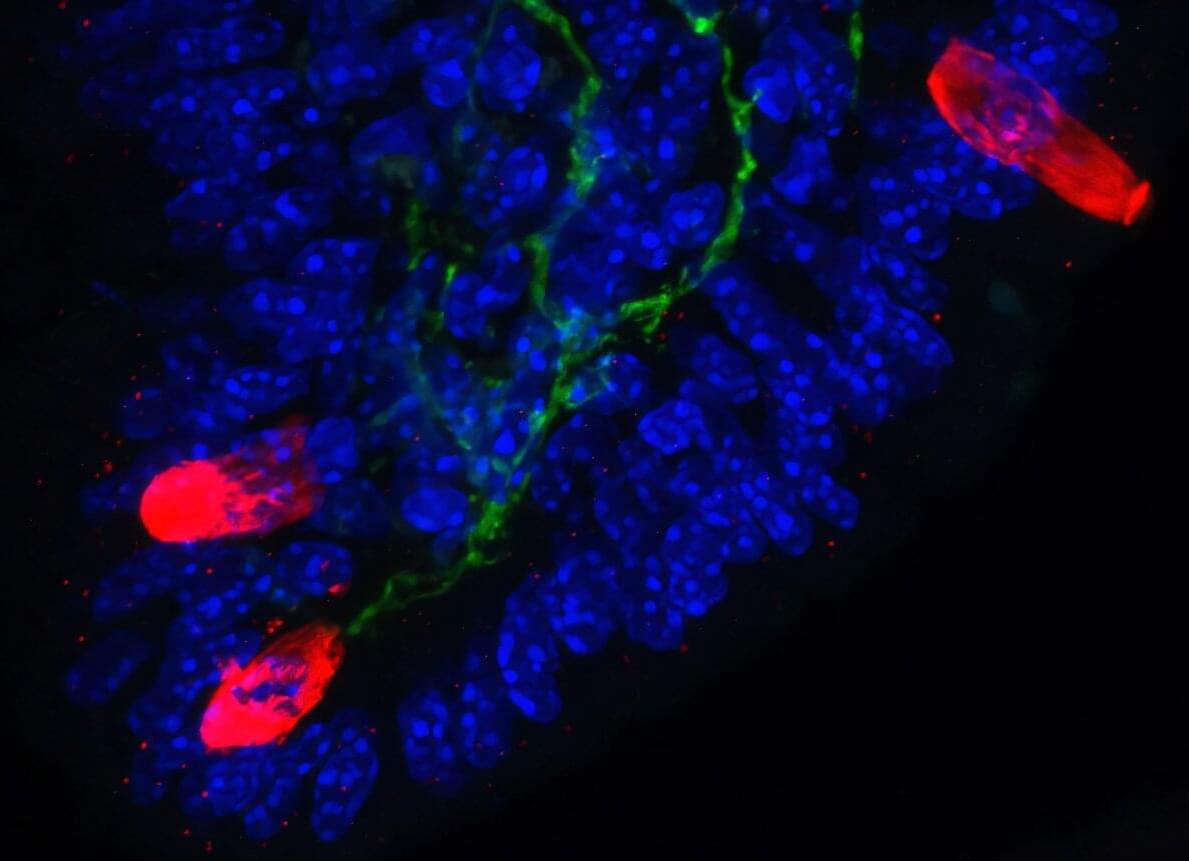
In a new study from Ian M. Mbano, Nuo Liu, Paul T. Elkington, Alex K. Shalek, Alasdair Leslie (University of KwaZulu-Natal) and colleagues, single-cell and spatial transcriptomics of human TB lung tissues from individuals in South Africa revealed that MMP1⁺CXCL5⁺ fibroblasts & SPP1⁺ macrophages are linked to TB disease & TB lung granuloma.
Ian M. Mbano, Nuo Liu, Marc H. Wadsworth, Mark J. Chambers, Thabo Mpotje, Osaretin E. Asowata, Sarah K. Nyquist, Kievershen Nargan, Duran Ramsuran, Farina Karim, Travis K. Hughes, Joshua D. Bromley, Robert Krause, Threnesan Naidoo, Liku B. Tezera, Michaela T. Reichmann, Sharie Keanne Ganchua, Henrik N. Kløverpris, Kaylesh J. Dullabh, Rajhmun Madansein, Sergio Triana, Adrie J.C. Steyn, Bonnie Berger, Mohlopheni J. Marakalala, Sarah M. Fortune, JoAnne L. Flynn, Paul T. Elkington, Alex K. Shalek, Alasdair Leslie; Single-cell and spatial profiling highlights TB-induced myofibroblasts as drivers of lung pathology. J Exp Med 2 March 2026; 223 : e20251067. doi: https://doi.org/10.1084/jem.20251067
Download citation file:
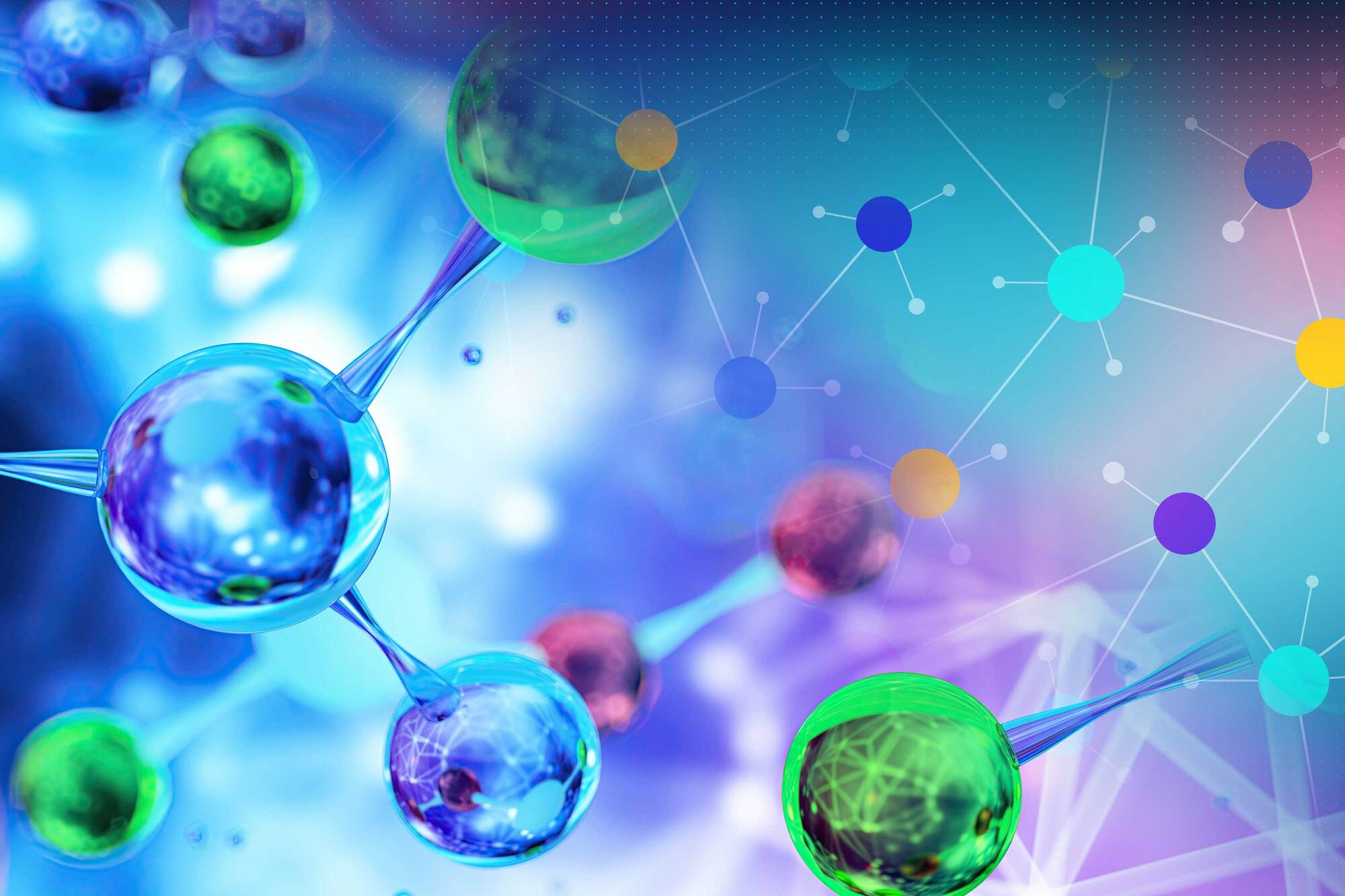
The study compared whole blood samples from 61 people meeting clinical diagnostic criteria for myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) with samples from healthy age-and sex-matched volunteers.
White blood cells from ME/CFS patients showed evidence of ‘energy stress’ in the form of higher levels of adenosine monophosphate (AMP) and adenosine diphosphate (ADP), indicating reduced generation of adenosine triphosphate (ATP), the key energy source within cells.
Profiling of immune cell populations revealed a trend toward less mature subsets of T-lymphocyte subsets, dendritic cells and natural killer cells in people with ME/CSF.
Comprehensive analysis of plasma proteins highlighted disruptions of vascular and immune homeostasis in patients with ME/CFS. Levels of proteins associated with activation of the endothelium – the innermost lining of blood vessels – and remodelling of vessel walls were higher, while levels of circulating immunoglobulin-related proteins were lower.
Although cellular energy dysfunction and altered immune profiles have been noted before in patients with ME/CFS, previous studies have often focused on a single analytical platform without looking at concurrence and interactions.
“ME/CFS is a complex disorder with undefined mechanisms, limited diagnostic tools and treatments,” said the senior author of the study. “Our findings provide further insights into the clinical and biological complexity of ME/CFS.”

Wearable technologies have the potential to transform gastrointestinal care by enabling continuous monitoring of activity in patients with cirrhosis and aiding in the early detection of hepatic encephalopathy. While these innovations provide valuable clinical insights, further efforts are needed to address challenges related to implementation and data management.
Current research into wearable technology in liver disease supports these possibilities. Studies of wrist-worn activity monitors have shown that reduced activity is associated with increased waitlist mortality among liver transplant candidates, as well as increased hospital admissions and mortality in patients with cirrhosis. Other investigations with wearables have linked sleep disturbances to poorer post-liver transplant outcomes and explored skin patches and transdermal sensors for detecting blood alcohol levels and inflammatory markers predictive of outcomes in cirrhosis, Buckholz said.
A major barrier to widespread implementation in clinical practices is the so-called “wearable paradox,” whereby early adopters of wearable technology tend to be relatively healthy, whereas those at highest risk are less likely to already use such devices, Buckholz noted. Increasing access, understanding, and uptake in vulnerable populations will therefore be critical.
Additional challenges include determining how to distill massive volumes of wearable data into concise formats that can be incorporated into electronic medical records (EMRs) and easily communicated to patients.
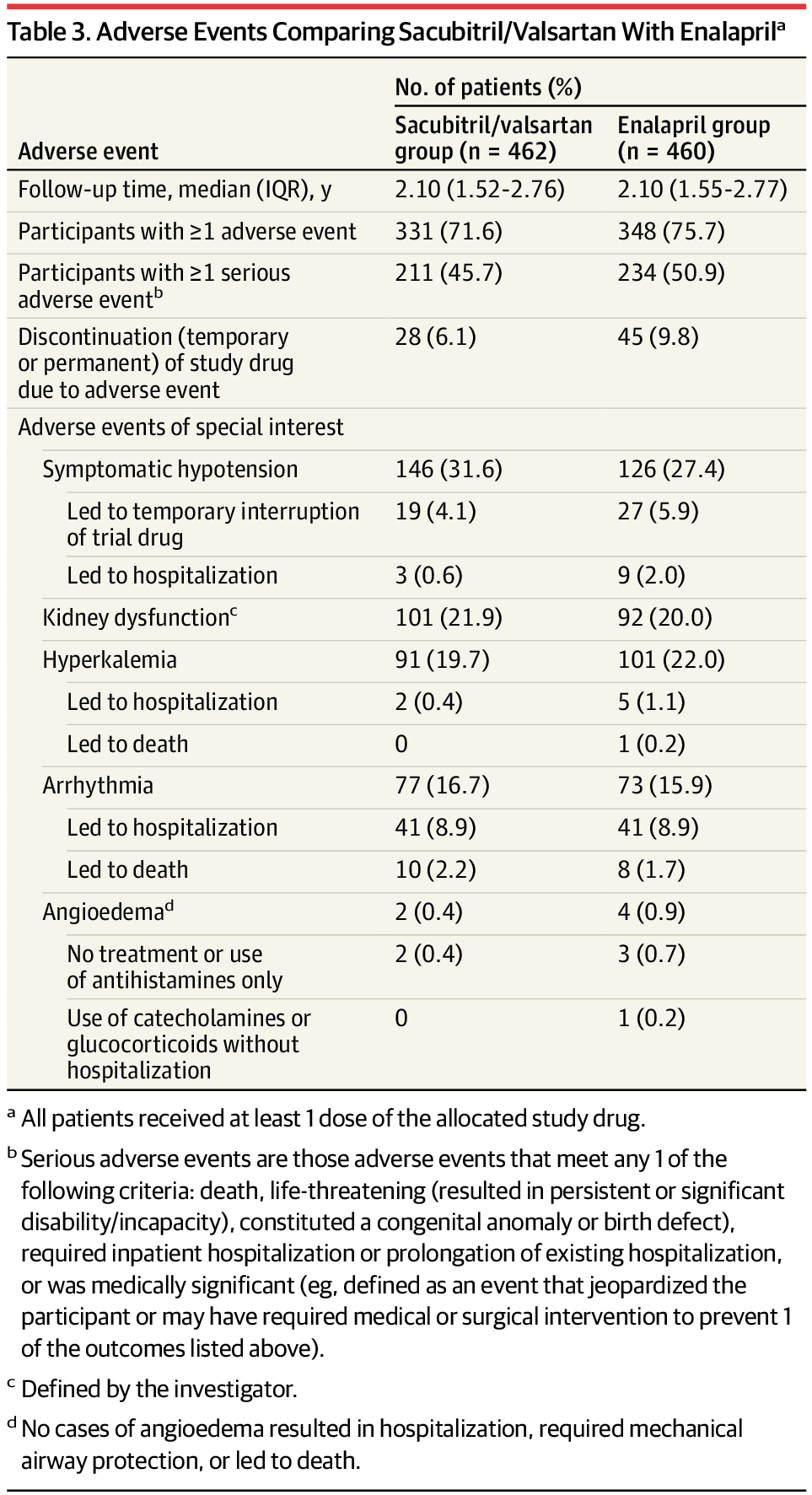
RCT: In patients with Chagas-related HFrEF, sacubitril/valsartan did not reduce rates of cardiovascular death or heart failure hospitalization compared with enalapril.
Although there was a greater reduction in NT-proBNP with sacubitril/valsartan, this did not impact observed clinical outcomes. These findings, in line with the BENEFIT trial, highlight the limited effect of biomarker improvements and antiparasitic therapy on clinical endpoints for Chagas disease.
The most common and severe complication of Chagas disease in its chronic phase is cardiomyopathy, which occurs in 30% to 40% of persons who are infected and can present as chronic myocarditis, conduction system abnormalities, cardioembolic episodes, heart failure (HF), and sudden death.5,11,12 Chagas cardiomyopathy is distinguished by its unique clinical features, including focal myocardial fibrosis, arrhythmogenicity, and ventricular aneurysm formation as well as a markedly high mortality rate, even in the absence of typical comorbidities.13 The reasons patients with HF due to Chagas disease have such a poor prognosis are not fully understood but may include persistent immune-mediated myocardial inflammation triggered by chronic parasitic infection, hypercoagulable state, right ventricular dysfunction, microvascular dysfunction, autonomic disturbance, high rates of ventricular arrhythmias, elevated risk of stroke, conduction disturbances, and ventricular aneurysm formation.5,13,14
Whether guideline-recommended medical therapies for HF are effective in patients with Chagas cardiomyopathy is unknown. No randomized clinical trial to date has been powered to test the efficacy and safety of any treatment in patients with HF caused by Chagas disease, and these patients were not adequately represented in pivotal HF trials.14 Although large randomized clinical trials are lacking, enalapril was selected as the comparator as a standard of care for HF management, including in patients with Chagas cardiomyopathy. The study by Szajnbok et al demonstrated that enalapril improved functional class and reduced heart size in patients with chronic Chagas heart disease, suggesting a beneficial hemodynamic effect.15 More recently, Penitente et al reported that enalapril reduced myocardial fibrosis and improved cardiac function in a murine model of chronic Chagas disease, supporting its role in modulating disease progression.16 Sacubitril/valsartan may offer incremental benefit over enalapril in patients with Chagas disease not only through neurohormonal and vasodilator effects but also by mitigating myocardial fibrosis and arrhythmias.14 Additionally, fully understanding the safety of HF treatments in this population is important, as these patients have more dysfunction of the right ventricle and lower blood pressure compared with other HF etiologies.14
Therefore, the PARACHUTE-HF (Prevention and Reduction of Adverse Outcomes in Chagasic Heart Failure Trial Evaluation) trial was designed to prospectively evaluate the efficacy and safety of the angiotensin receptor-neprilysin inhibitor sacubitril/valsartan in patients with HF with reduced ejection fraction (HFrEF) caused by Chagas disease.
Pain-sensing neurons in the gut kindle inflammatory immune responses that cause allergies and asthma, according to a new study by Weill Cornell Medicine. The findings, published in Nature, suggest that current drugs may not be as effective because they only address the immune component of these conditions, overlooking the contribution of neurons.
“Today’s blockbuster biologics are sometimes only 50% effective and when the treatments do work, they sometimes lose their efficacy over time,” said senior author Dr. David Artis, director of the Jill Roberts Institute for Research in Inflammatory Bowel Disease and the Michael Kors Professor in Immunology at Weill Cornell.
While the idea may be new to the field, Dr. Artis has been thinking about the role the nervous system may play in allergies and asthma for about two decades. For example, many of the symptoms that characterize these conditions, like itching and wheezing, are known to be neuronally controlled. “That was one of the clues that prompted us to look closer for a connection,” Dr. Artis said.
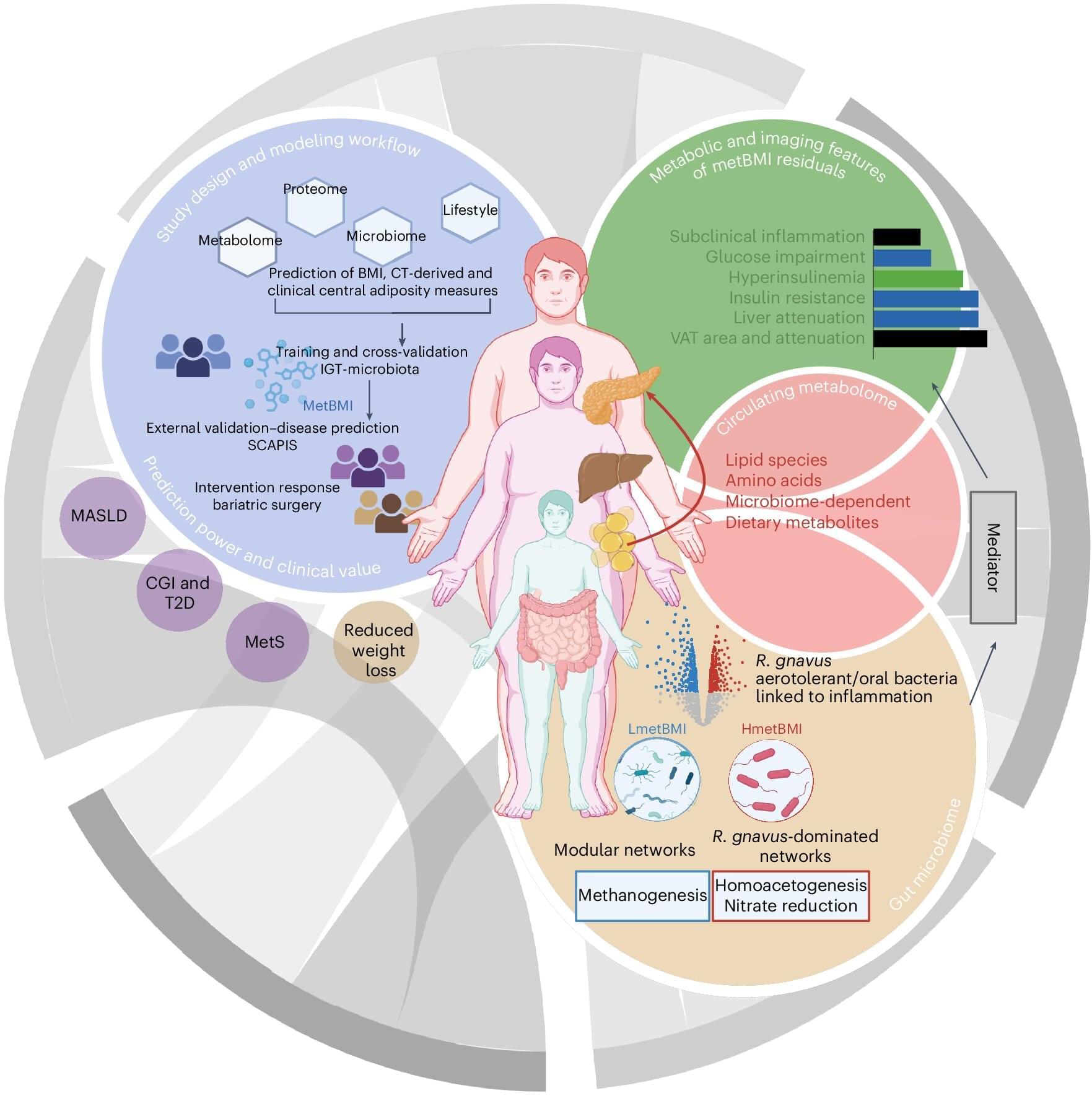
Researchers at Leipzig University and the University of Gothenburg have developed a novel approach to assessing an individual’s risk of metabolic diseases such as diabetes or fatty liver disease more precisely. Instead of relying solely on the widely used body mass index (BMI), the team developed an AI-based computational model using metabolic measurements. This so-called metabolic BMI shows that people of normal weight with a high metabolic BMI have up to a fivefold higher risk of metabolic disease. The findings have been published in the journal Nature Medicine.
The conventional body mass index, calculated using height and weight, may indicate overweight but does not reflect how healthy or unhealthy body fat actually is. According to BMI classifications, up to 30% of people are considered to be of normal weight but already show dangerous metabolic changes. Conversely, there are individuals with an elevated BMI whose metabolism remains largely unremarkable. This discrepancy can lead to at-risk patients being identified and treated too late.
For the current scientific study, the international research team analyzed data from two large Swedish population studies involving a total of almost 2,000 participants. In addition to standard health and lifestyle parameters, extensive laboratory data from blood samples and analyses of the gut microbiome were collected. Based on this dataset, the researchers developed a computational model that predicts metabolic BMI.

Their in-depth DNA analysis also showed that resident killer whales shared the same haplotype (group of inherited genes) while the transients had eight different haplotypes making them more genetically diverse. This finding suggests that transient killer whales used Hokkaido as a refuge during the last Ice Age, the researchers say.
“Clarifying the ecological characteristics of killer whales is crucial for achieving coexistence with them,” says first author Momoka Suzuki, Kyoto University, in a statement.
Understanding the diet and behaviour of orcas in Japanese waters gives conservationists important information that can help protect the animals from threats. “They are deeply entwined with human activities such as tourism and fisheries in Hokkaido,” adds Suzuki.