Research is first initiative from Big Tech group’s AI health unit formed by ex-DeepMind co-founder Mustafa Suleyman.


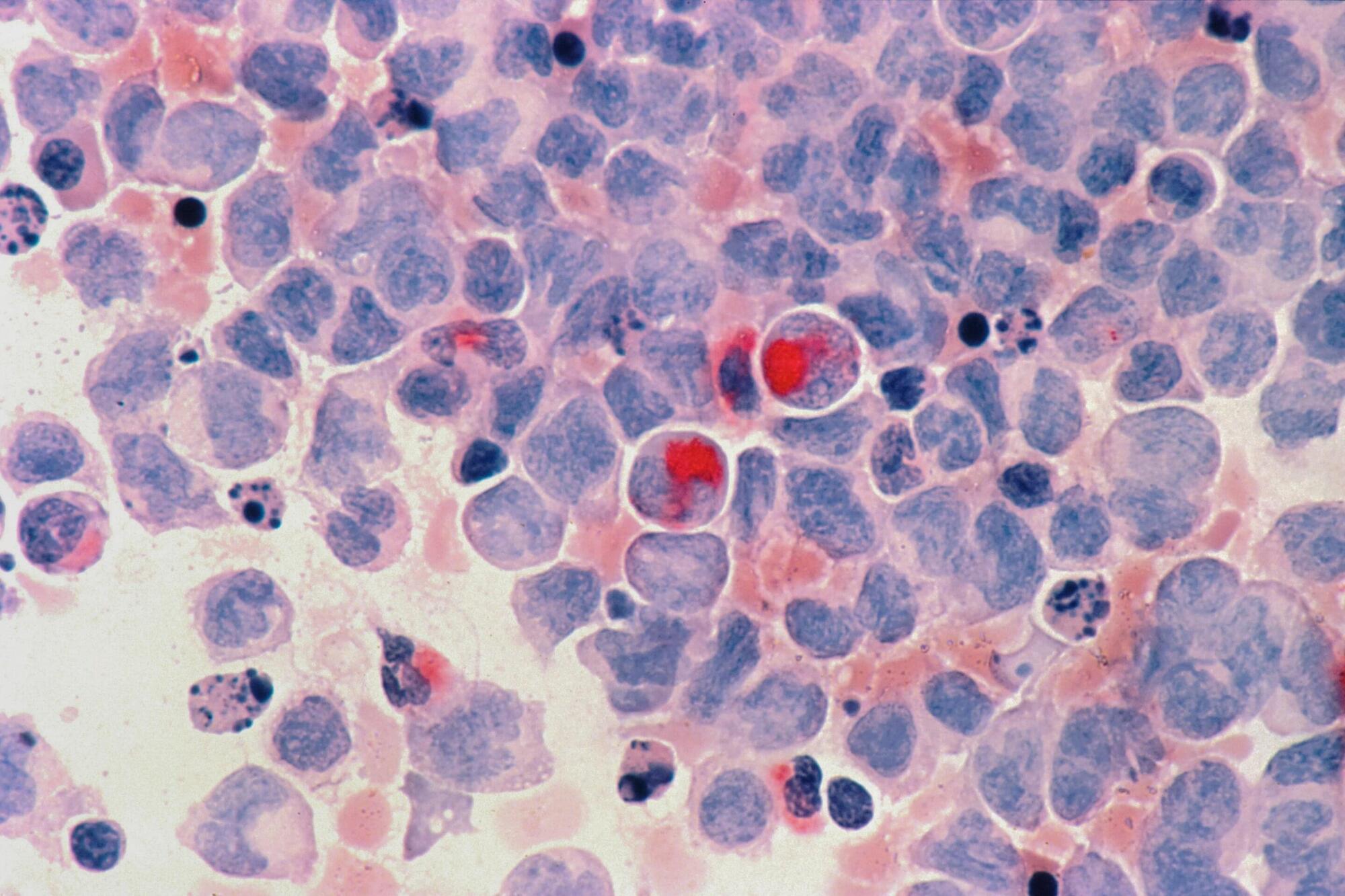
Researchers working on an incurable blood cancer can now use a new lab model that could make testing potential new treatments and diagnostics easier and quicker, new research has found.
In a paper published in Nature Communications, a team of researchers led by the University of Birmingham has studied blood cells from patients with a blood cancer called myelodysplastic syndrome disease (MDS). This disease often develops into a highly aggressive form of acute myeloid leukemia (AML).
Working with this new model has led to confirmation that a mutation in the gene CEBPA causes progression from MDS to AML.
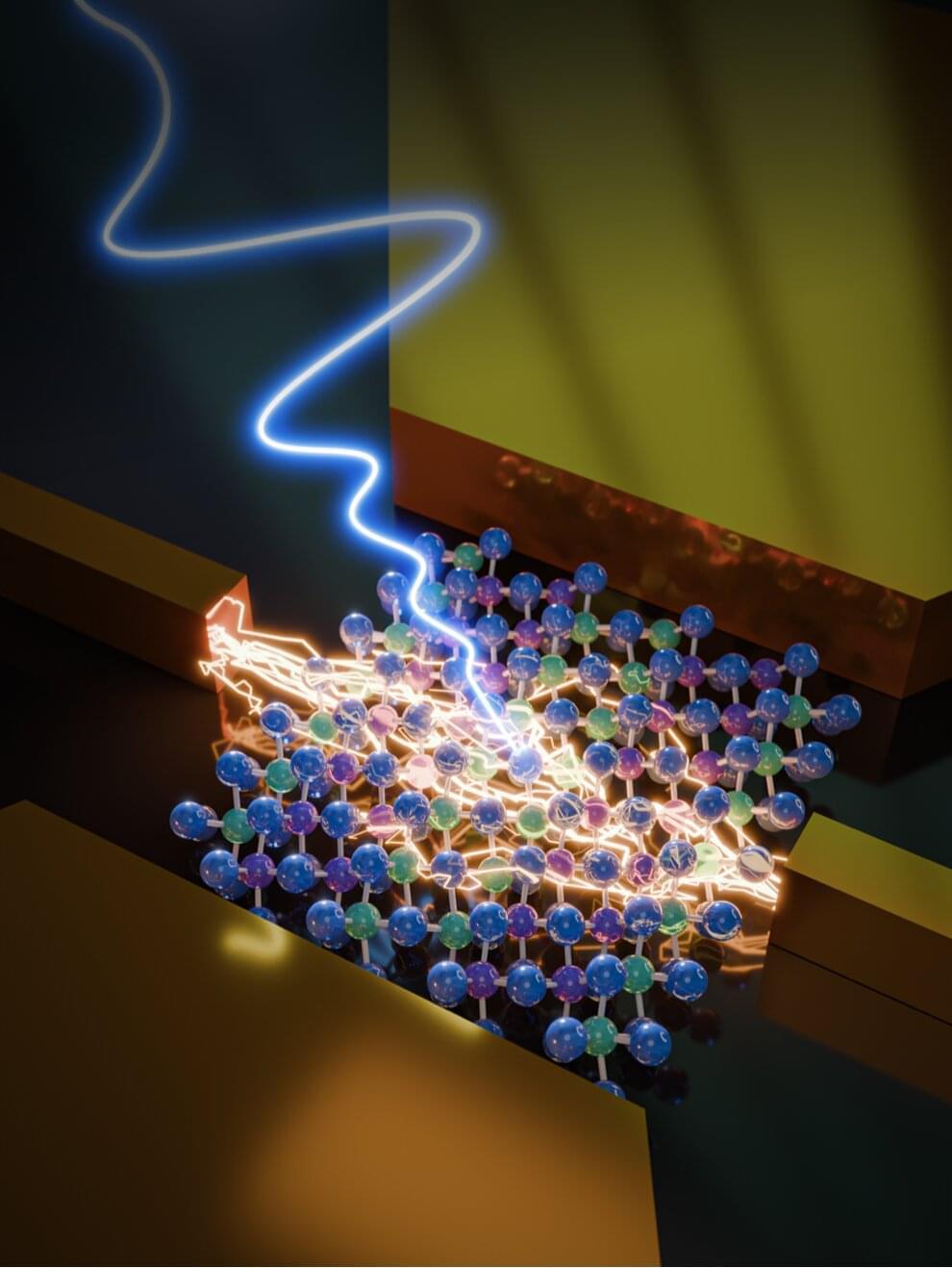
Terahertz radiation (THz), electromagnetic radiation with frequencies ranging between 0.1 and 10 THz, could be leveraged to develop various new technologies, including imaging and communication systems. So far, however, a lack of fast and sensitive detectors that can detect radiation across a wide range of frequencies has limited the development of these THz-sensing technologies.
In a recent paper published in Nature Electronics, researchers at the University of Wisconsin-Madison, the University of Tennessee and other institutes have introduced new photodetectors made of tantalum iridium telluride (TaIrTe₄), a 2D-correlated topological semimetal that exhibits advantageous properties. Most notably, this material exhibits a strong nonlinear Hall effect, a physical effect that entails a transverse voltage in the absence of an external magnetic field, which is nonlinearly proportional to an applied electric field or current.
“THz technology is critical in quantum information technology and biomedical sensing because its frequency resonates with low-energy collective excitations in quantum materials and molecular vibrations in biological matters,” Jun Xiao, senior author of the paper, told Phys.org.

Germline cells play a key role in the transmission of phenotypes and physiological adaptations to subsequent generations (1). Over a century ago, August Weismann proposed that changes in somatic cells cannot be passed on to germ cells or offspring, a theory known as the Weismann barrier (2). Nevertheless, recent studies have proven that the Weismann barrier is permeable, and information can pass from soma to germline and modulate offspring phenotypes. In the past decade, there has been tremendous interest and progress in understanding how an altered microbiome (dysbiosis) affects different somatic cells that compose body tissues, such as brain, liver, heart, kidney, and lungs (3). Nevertheless, whether gut microbiome dysbiosis can exert an influence on the mammalian germline cells (i.e., gut to germline), and ultimately nonexposed offspring, remains unclear.
To tackle this research question, my colleagues and I established an inducible model of gut microbiota dysbiosis in isogenic male mice, using ad lib nonabsorbable antibiotics (nABX) that cannot cross the epithelial barrier of the gut (4). As expected, 6 weeks of low-dose nABX treatment led to a physiologically significant dysbiosis, which is reversible and gradually normalized to a physiologically healthy gut microbiota after 8 weeks of nABX withdrawal (6 weeks + 8 recovery). The induced dysbiosis after 6 weeks of nABX had no appreciable effects on male body weight, growth, or fertility. No nABx residues were detected in the serum or testes of treated males, which confirmed that any distal tissue responses are gut dysbiosis–induced rather than systemic drug effects.
We then examined physiological changes in the male reproductive system in response to 6 weeks of dysbiosis. Dysbiotic males had smaller testes, lower sperm count, and more abnormally shaped sperm. Histological analysis uncovered a wide range of anatomical abnormalities in testes of dysbiotic males, including increased number of abnormal seminiferous tubules, reduced epithelial thickness, and absence of mitotic compartments, which were not observed in control testes. Testicular metabolomic profiles revealed that testes clustered according to gut microbiota status and exhibited dysregulated sphingolipids, glycerophospholipids, and endocannabinoids, all known to play pivotal roles in germ cell function. Moreover, in dysbiotic male testes, spermatogenesis-regulating genes were misexpressed—most notably leptin, a reproductive hormone, was strongly down-regulated.
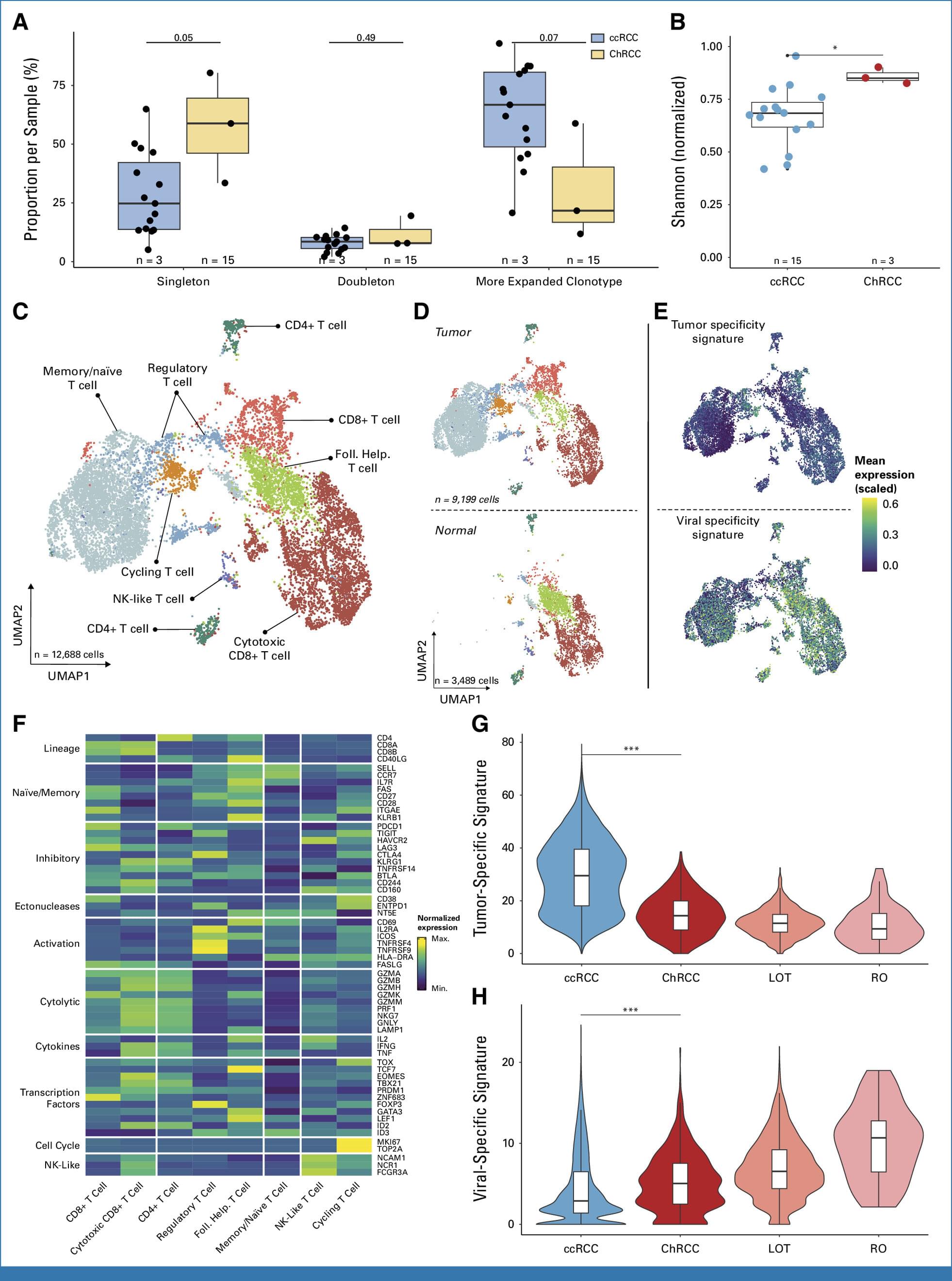
Cancer-fighting T-cells, the immune system’s primary enforcers, are scarce in the rare kidney cancer called chromophobe renal cell carcinoma (ChRCC) and those that are present are indifferent to the tumor threat and traditional immune therapies, revealing the need for new targets and treatments.
Those are among the results described in a July 2 published report in the Journal of Clinical Oncology that set out to understand the biology of certain kidney tumors, including ChRCC, and their immune responses.
The study found that ChRCC, which accounts for about 5% of all kidney cancers, has fewer T-cells and key molecules required for an immune response than other kidney cancers and poorer response and survival rates when treated with immune-based therapies. Other examined kidney tumors included in the study were low-grade oncocytic tumor (LOT) and the usually benign renal oncocytoma (RO).
DNA sequencing shows young trees are more likely to have gene variants that confer partial resistance to a fungus that has been wiping out ash trees across Europe
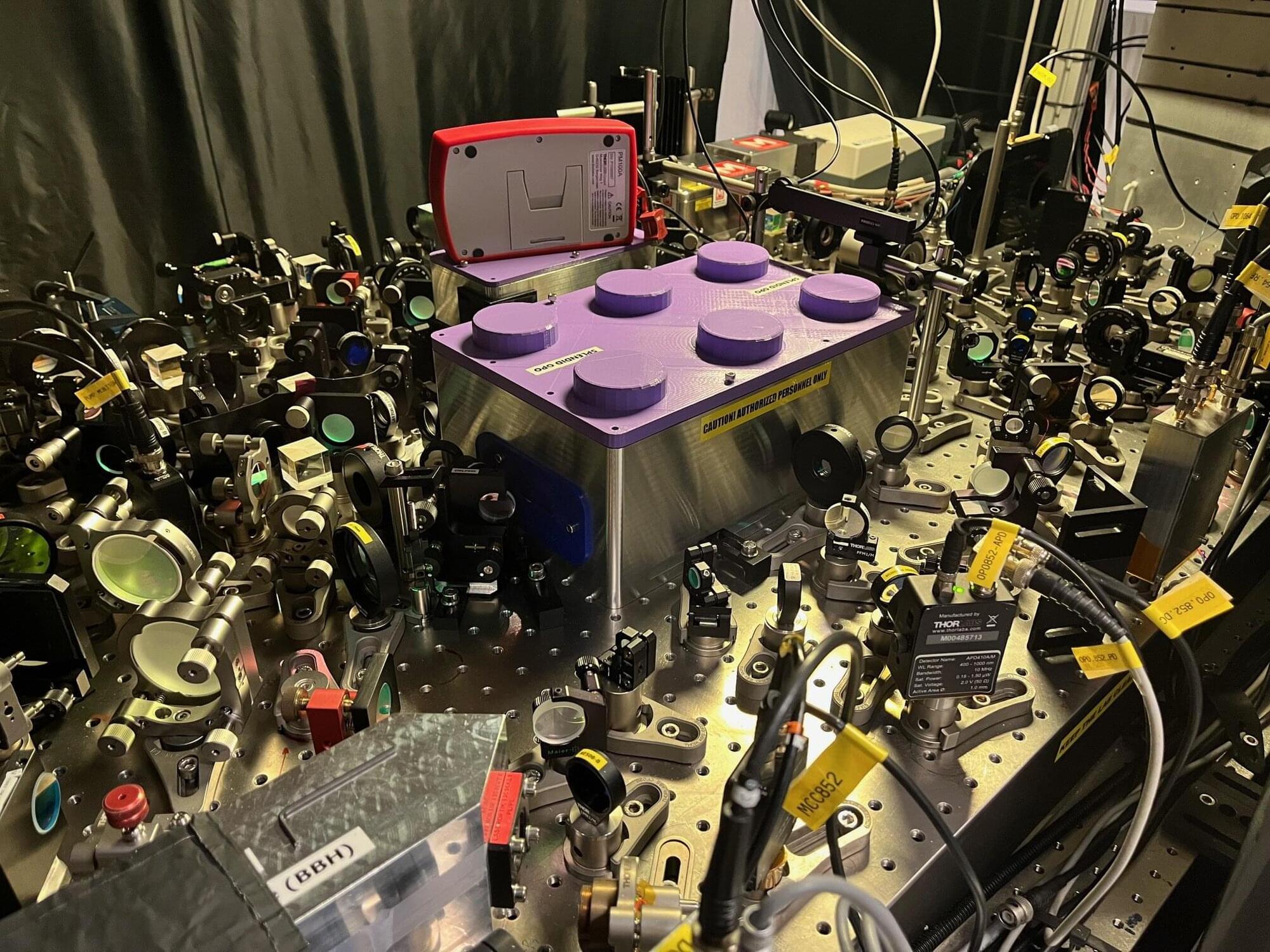
Researchers at the Niels Bohr Institute, University of Copenhagen, have developed a tunable system that paves the way for more accurate sensing in a variety of technologies, including biomedical diagnostics. The result is published in Nature.
The potential range of technologies is large, stretching from the largest to smallest scales, from detecting gravitational waves in space to sensing the tiny fluctuations in our own bodies.
Optical sensing technologies are already part of everyday life. In recent years, advances in quantum optics have pushed the sensitivity of these devices closer to the so-called standard quantum limit—a practical boundary that arises from the inevitable noise arising from measuring on the smallest scales.
When the first reports of a new COVID-19 variant emerge, scientists worldwide scramble to answer a critical question: Will this new strain be more contagious or more severe than its predecessors? By the time answers arrive, it’s frequently too late to inform immediate public policy decisions or adjust vaccine strategies, costing public health officials valuable time, effort, and resources.
In a pair of recent publications in Proceedings of the National Academy of Sciences, a research team in the Department of Chemistry and Chemical Biology combined biophysics with artificial intelligence to identify high-risk viral variants in record time—offering a transformative approach for handling pandemics. Their goal: to get ahead of a virus by forecasting its evolutionary leaps before it threatens public health.
“As a society, we are often very unprepared for the emergence of new viruses and pandemics, so our lab has been working on ways to be more proactive,” said senior author Eugene Shakhnovich, Roy G. Gordon Professor of Chemistry. “We used fundamental principles of physics and chemistry to develop a multiscale model to predict the course of evolution of a particular variant and to predict which variants will become dominant in populations.”
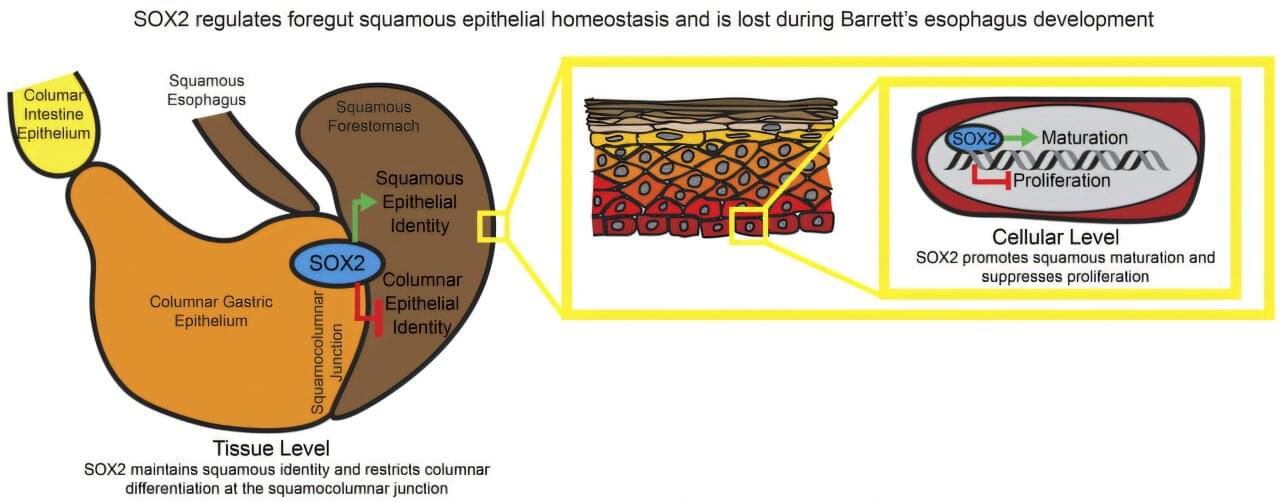
A team led by researchers at Baylor College of Medicine and Washington University School of Medicine has shed light on the process that drives Barrett’s esophagus formation. This condition affects the lining of the esophagus—the tube that carries food from the mouth to the stomach—and increases the risk of developing esophageal adenocarcinoma, a serious and often deadly cancer.
The study, published in the Journal of Clinical Investigation, reveals that two important genes involved in guiding and maintaining the identity of the esophagus and intestine, SOX2 and CDX2, are altered in Barrett’s esophagus. The findings not only deepen our understanding of how the disease develops but also open the door to new ways of identifying people at risk and potentially preventing the condition from progressing to cancer.
“Esophageal adenocarcinoma is one of the fastest growing solid cancers. It is difficult to treat, and there are no effective screening techniques available,” said first and co-corresponding author Dr. Ramon Jin, assistant professor in the John T. Milliken Department of Medicine at Washington University.
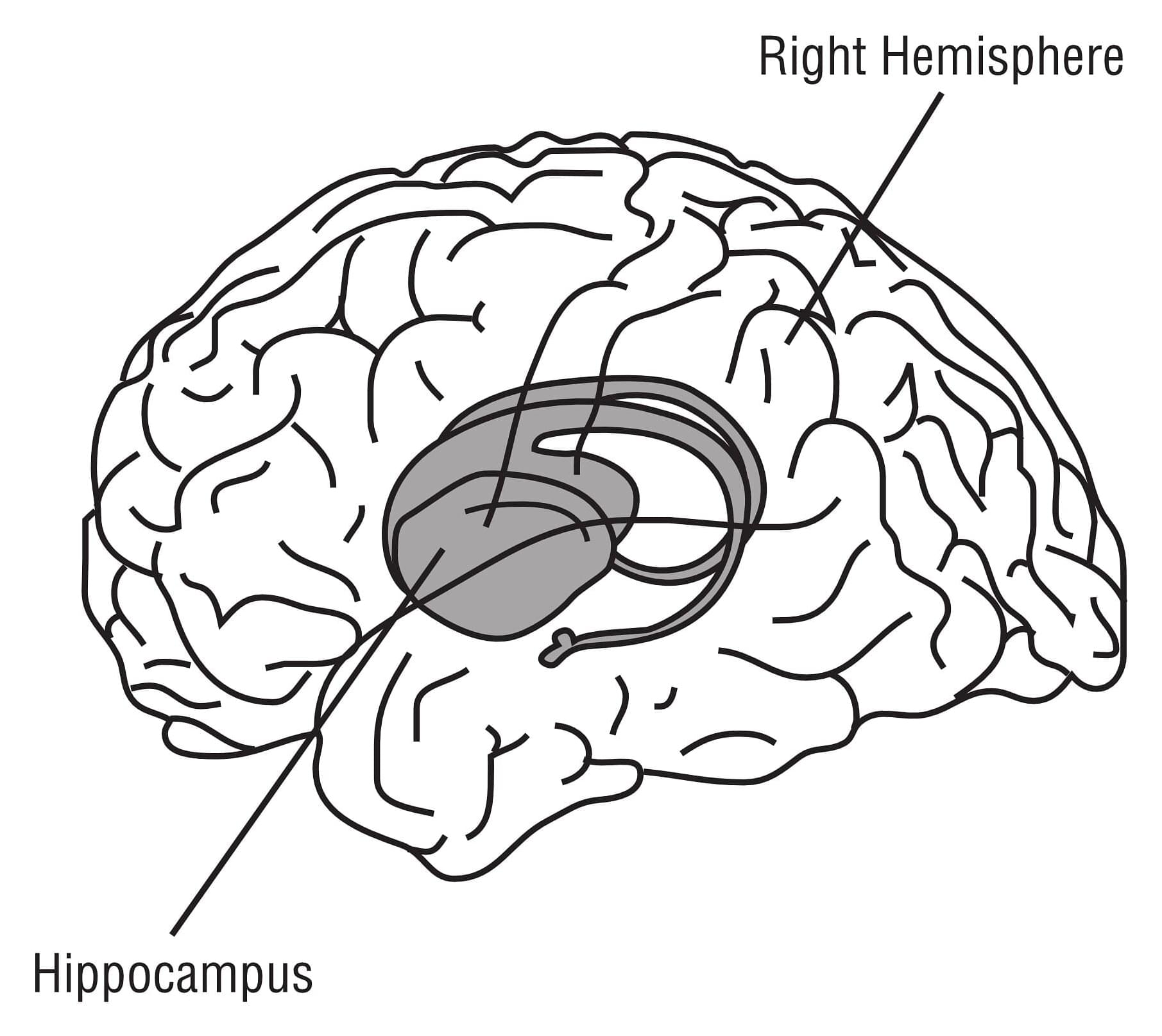
A study in the journal Science presents compelling new evidence that neurons in the brain’s memory center, the hippocampus, continue to form well into late adulthood. The research from Karolinska Institutet in Sweden provides answers to a fundamental and long-debated question about the human brain’s adaptability.
The hippocampus is a brain region that is essential for learning and memory and involved in emotion regulation. Back in 2013, Jonas Frisén’s research group at Karolinska Institutet showed in a high-profile study that new neurons can form in the hippocampus of adult humans. The researchers then measured carbon-14 levels in DNA from brain tissue, which made it possible to determine when the cells were formed.