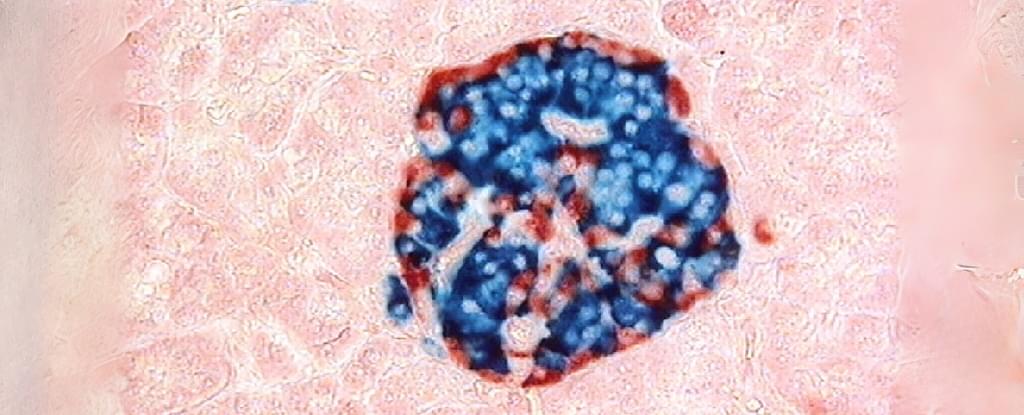
A dozen volunteers with severe type 1 diabetes showed clear improvements in their condition 12 months after receiving a revolutionary stem cell treatment, with all but two dropping their insulin therapy altogether.


The COVID-19 pandemic yielded important advances in testing for respiratory viruses, but it also exposed important unmet needs in screening to prevent the spread of infections in high-risk settings.
While PCR (polymerase chain reaction) tests are the gold standard for detecting viral infections, they remain a challenge for screening large numbers of people in places vulnerable to outbreaks—such as health care centers and nursing homes—due to high costs and the fact that different tests are required for each virus.
A new Yale study, however, finds that an alternate strategy—using a nasal swab to screen for an antiviral protein produced by the body as a defense against infection—can be an effective method for ruling out respiratory infections, limiting PCR testing only to those most likely to be infected, at a fraction of the cost.
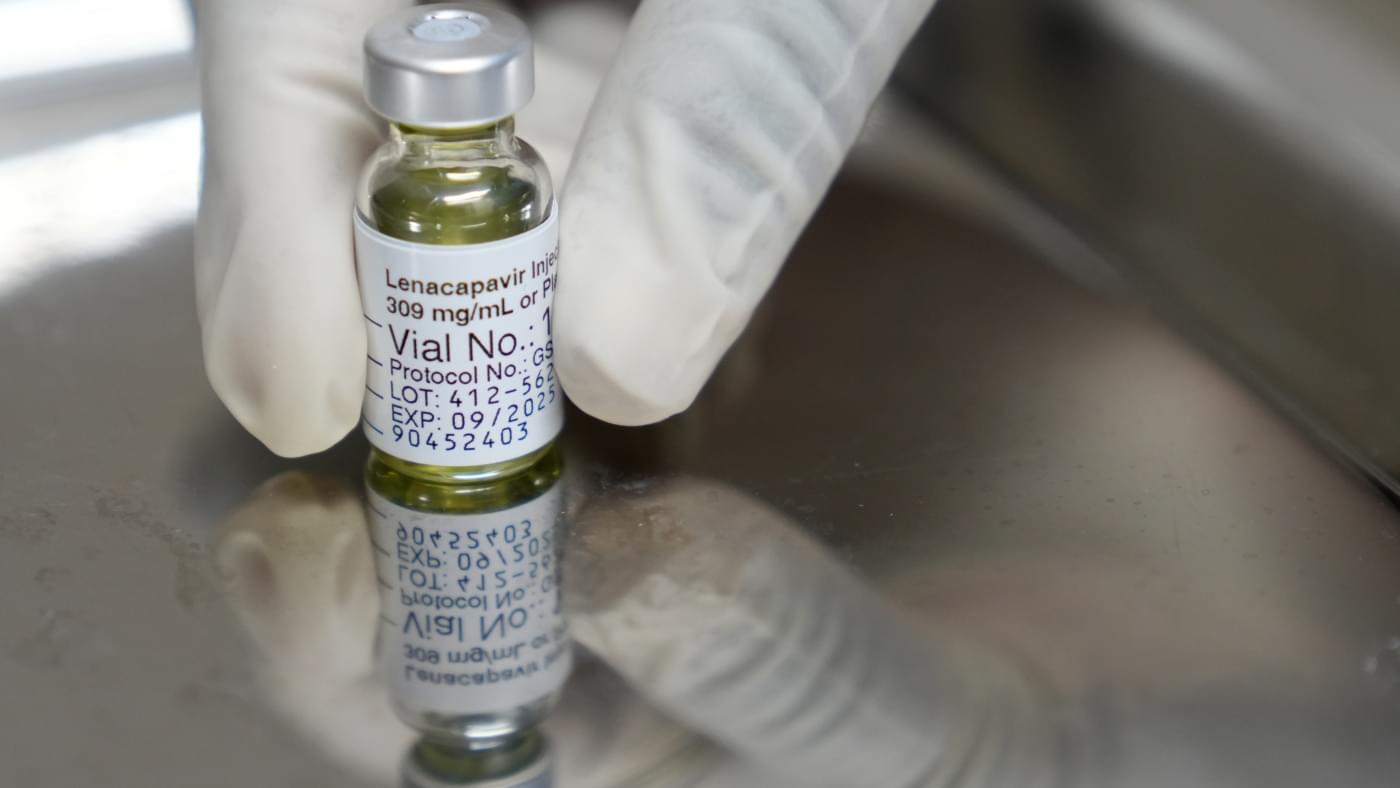
Researchers at the University of California, Irvine have successfully performed preclinical laboratory testing of a replacement heart valve intended for toddlers and young children with congenital cardiac defects, a key step toward obtaining approval for human use. The results of their study were published recently in the Journal of the American Heart Association.
The management of patients with congenital heart disease who require surgical pulmonary valve replacement typically occurs between the ages of 2 and 10. To be eligible for a minimally invasive transcatheter pulmonary valve procedure, patients currently must weigh at least 45 pounds. For children to receive minimally invasive treatment, they must be large enough so that their veins can accommodate the size of a crimped replacement valve.
The Iris Valve, designed and developed by the UC Irvine team, can be implanted in children weighing as little as 17 to 22 pounds and gradually expanded to an adult diameter as they grow.
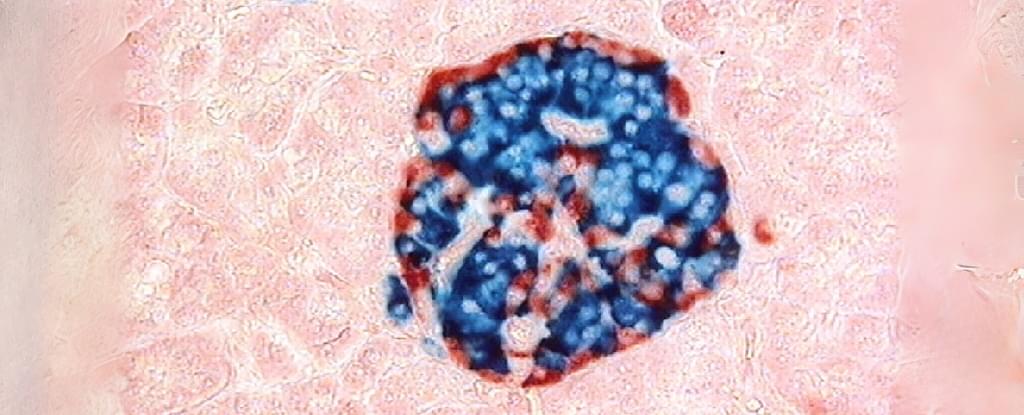
A novel PET imaging approach has revealed distinct patterns of brain inflammation in patients with progressive apraxia of speech (PAOS), a rare neurodegenerative disorder that affects speech planning. These findings provide new insight into how neuroinflammation and tau pathology may drive disease progression in PAOS, opening potential avenues for earlier diagnosis and targeted treatments.
This research was presented at the Society of Nuclear Medicine and Molecular Imaging 2025 Annual Meeting and published as a supplement in the Journal of Nuclear Medicine.
PAOS is a neurodegenerative disorder that impairs the brain’s ability to plan and coordinate speech. It is marked by a slow speaking rate, distorted sounds, and effortful facial movements during speech. Patients with PAOS are likely to have Parkinson-plus syndrome in the later stages, meeting criteria for progressive supranuclear palsy or corticobasal syndrome, and typically have a 4-repeat tauopathy at autopsy.

Insulin resistance detected by routine triglyceride-glucose (TyG) index can flag people with early Alzheimer’s who are four times more likely to present rapid cognitive decline, according to new research presented at the European Academy of Neurology (EAN) Congress 2025.
Neurologists at the University of Brescia reviewed records of 315 non-diabetic patients with cognitive deficits, including 200 with biologically confirmed Alzheimer’s disease. All subjects underwent an assessment of insulin resistance using the TyG index and a clinical follow-up of three years.
The work is published in the journal Alzheimer’s & Dementia.