We’re not wired to feel safe all the time, but maybe one day we could be.
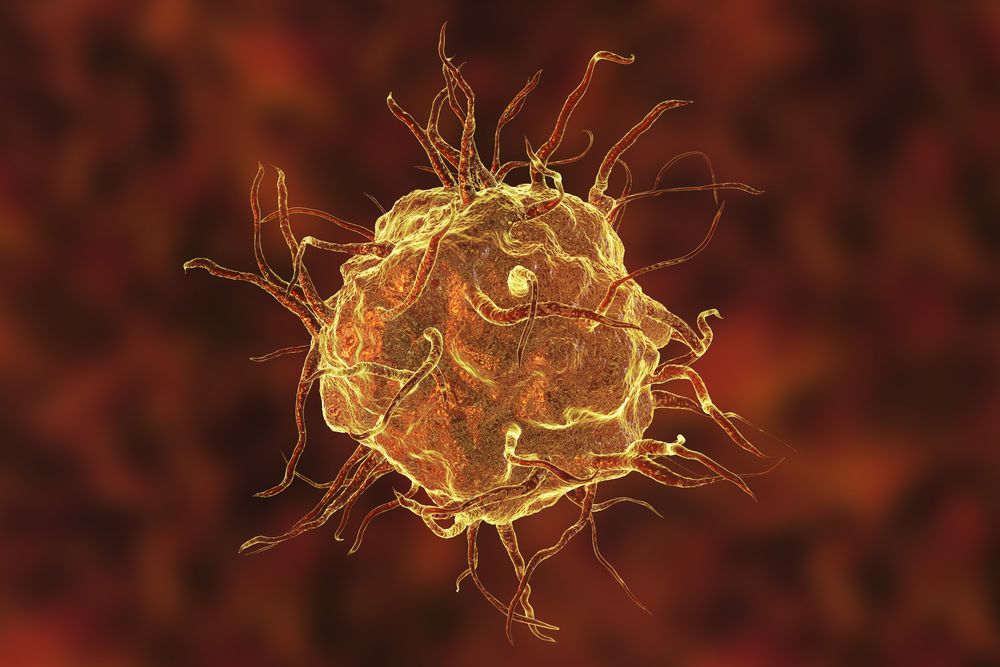
A new study investigating the neurological basis of anxiety in the brain has identified ‘anxiety cells’ located in the hippocampus – which not only regulate anxious behaviour but can be controlled by a beam of light.
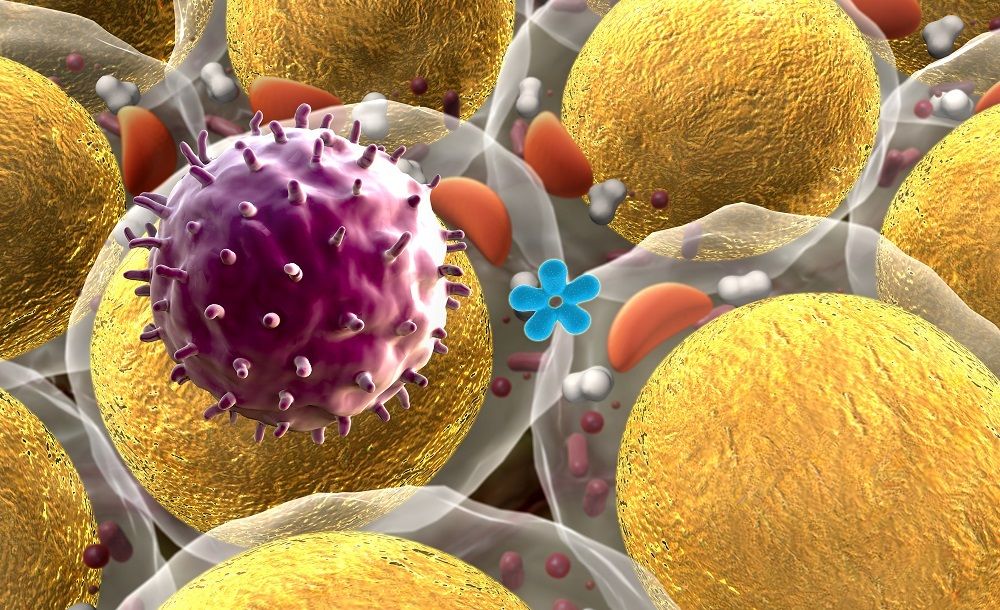
The findings, so far demonstrated in experiments with lab mice, could offer a ray of hope for the millions of people worldwide who experience anxiety disorders (including almost one in five adults in the US), by leading to new drugs that silence these anxiety-controlling neurons.