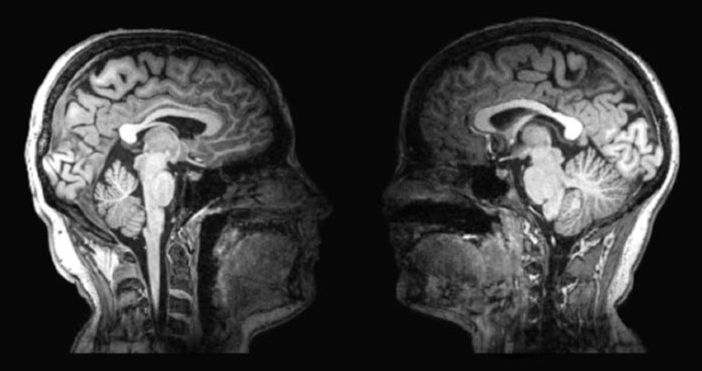
“An international study involving Monash physicists has cornered a new approach to measure consciousness, potentially changing our understanding of complex neurological problems.
The study published today in Physical Review Research describes how tools from physics and complexity theory were used to determine the level of consciousness in fruit flies.
“This is a major problem in neuroscience, where it is crucial to differentiate between unresponsive vegetative patients and those suffering from a condition in which a patient is aware but cannot move or communicate verbally because of complete paralysis of nearly all voluntary muscles in the body,” said study author Dr. Kavan Modi, from the Monash University School of Physics and Astronomy.”
An international study involving Monash physicists has conrmed a new approach to measure consciousness, potentially changing our understanding complex neurological problems.
DOI: 10.1103/PhysRevResearch.2.023219
Organisation/s: Monash University.