“Once they are ingested, up to 90% of the plastic fragments that reach the intestine are excreted. However, one part is fragmented into nanoplastics which are capable, due to their small size and molecular properties, to penetrate the cells and cause harmful effects. The study establishes that alterations in food absorption have been described, as well as inflammatory reactions in the intestinal walls, changes in the composition and functioning of the gut microbiome, effects on the body’s metabolism and ability to produce, and lastly, alterations in immune responses. The article alerts about the possibility of a long-term exposure to plastic, accumulated throughout generations, could give way to unpredictable changes even in the very genome, as has been observed in some animal models.”
We live in a world invaded by plastic. Its role as a chemically stable, versatile and multi-purpose fostered its massive use, which has finally translated into our current situation of planetary pollution. Moreover, when plastic degrades it breaks into smaller micro and nanoparticles, becoming present in the water we drink, the air we breathe and almost everything we touch. That is how nanoplastics penetrate the organism and produce side effects.
A revised study led by the Universitat Autónoma de Barcelona (UAB), the CREAF and the Centre for Environmental and Marine Studies (CESAM) at the University of Aviero, Portugal, and published in the journal Science Bulletin, verifies that the nanoplastics affect the composition and diversity of our intestinal microbiome and that this can cause damage to our health. This effect can be seen in both vertebrates and invertebrates, and has been proved in situations in which the exposure is widespread and prolonged. Additionally, with alteration of the gut microbiome come alterations in the immune, endocrine and nervous system and therefore, although not enough is known about the specific physiological mechanisms, the study alerts that stress to the gut microbiome could alter the health of humans.
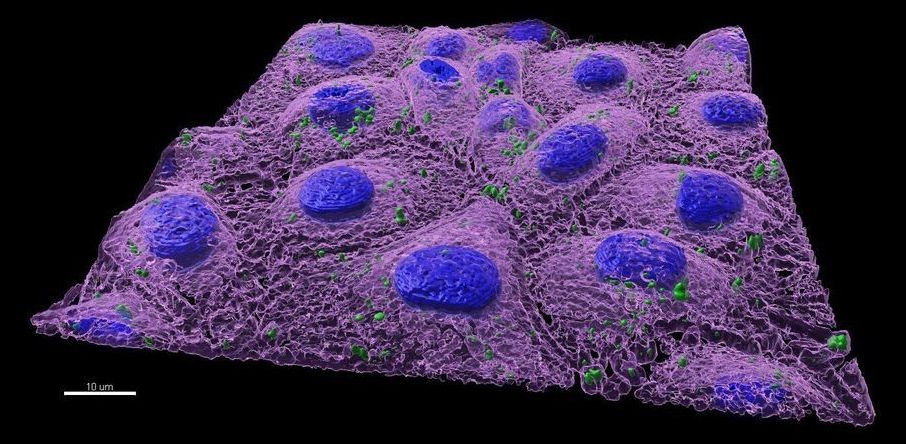
The health effects of being exposed to nanoplastics was traditionally evaluated in aquatic animals such as molluscs, crustaceans and fish. Recent in vitro analyzes, using cell cultures of fish and mammals, has allowed scientists to analyze the changes in gene expression associated with the presence of nanoplastics from a toxicological viewpoint. The majority of neurological, endocrine and immunological tracts in these vertebrates are very similar to those of humans, and therefore authors warn that some of the effects observed in these models could also be applied to humans. Understanding and analyzing the process through which these plastic fragments penetrate the organism and harm it is fundamental, as is determining precisely the amount and typology of nanoplastics polluting the environment.