By blocking a receptor in macrophages, researchers were able to reverse aging in mice.
There are many suggested causes of old age. Telomere shortening, DNA damage, and depletion of stem cells are just a few of the proposed sources.
Recently, researchers found that a type of cell called a macrophage also plays a crucial role in aging. Macrophages are phagocytotic immune cells; they consume cells and other pathogens flagged by the immune system as dangerous. When macrophages need to consume a pathogen, their energy needs drastically go up.
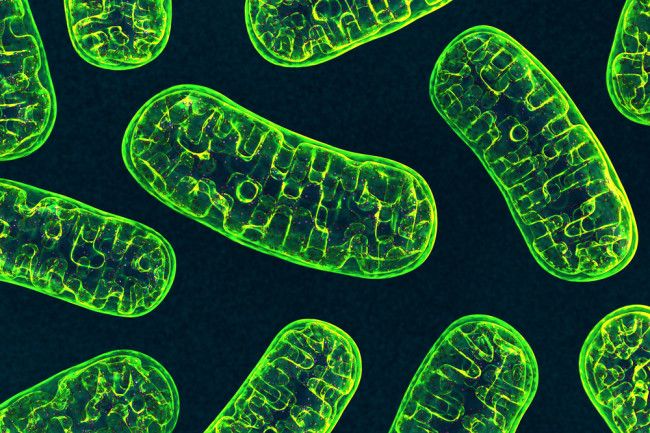
Remember in biology when you were told that the mitochondria was the “powerhouse of the cell?” Cells produce energy through two main ways: glycolysis and oxidative phosphorylation. Both of these processes work inside the mitochondria by converting glucose into ATP, a molecule that acts cell’s “currency” on energy. Glycolysis converts glucose to ATP by degrading glucose into pyruvate. This reaction triggers the production of 2 ATP per molecule of glucose, which allows the cell can then use for other biological functions. Oxidative phosphorylation, on the other hand, is far more complicated, but also yields much more ATP. In a nutshell, it strips the electrons from hydrogen molecules so it can create an electrical gradient and produce up to 38 ATP per glucose molecule. Researchers found that as macrophages age, they tend to shut down these “metabolic pathways,” as they are called.