Interview with a very important researcher who gives a reality check on a few things (Sirtuins) and explains how effective Rapamycin has been.
Professor Matt Kaeberlein discusses aspects of aging and proposed interventions to improve health. He gives an in-depth review on sirtuins, resveratrol, fasting, NAD precursors, and rapamycin.
Timestamps.
0:00 Intro.
0:25 Discovery of Sirtuins.
7:30 Resveratrol & Health.
11:05 Calorie Restriction & Fasting.
17:07 What Is A Healthy Diet?
21:46 NAD+ Precursors.
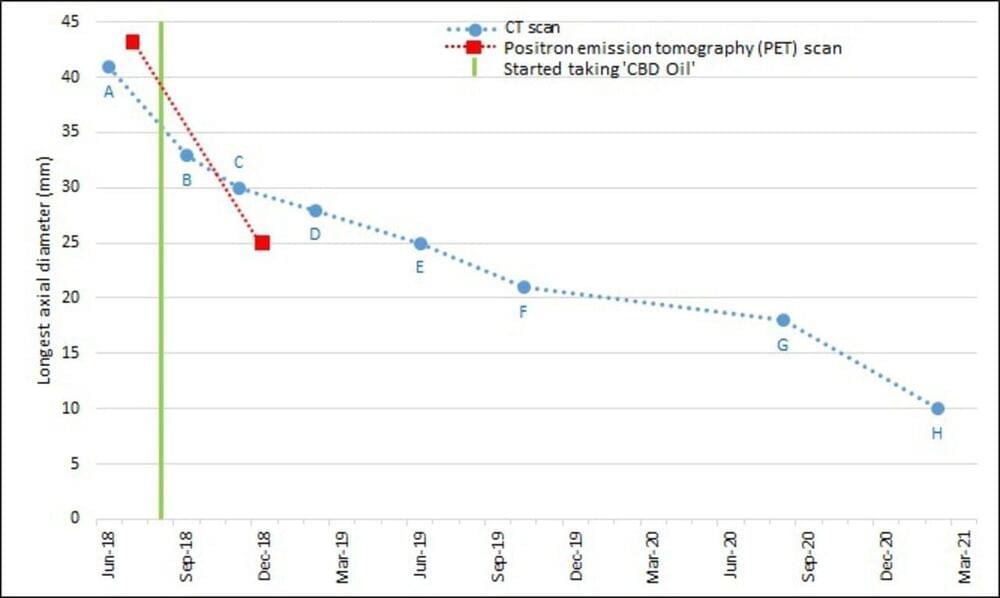
29:07 Rapamycin & Lifespan.
32:50 Rapamycin & Dog Aging Project.
38:45 Intermittent Fasting In Dogs.
40:45 Rapamycin Human Clinical Studies.
50:30 DNA Methylation Clocks.
54:15 What Areas Are Exciting For Healthspan Extension?
56:25 Yamanaka Factors.
59:55 How Do We Avoid Hype Over Substance?
1:06:50 Senolytics.
1:17:36 What Supplements Does Professor Kaeberlein Take?
My full supplement stack: http://bit.ly/39vRnXX
Supplements I source from Amazon: http://amzn.to/3o2ULOV
✨10% Discounts✨