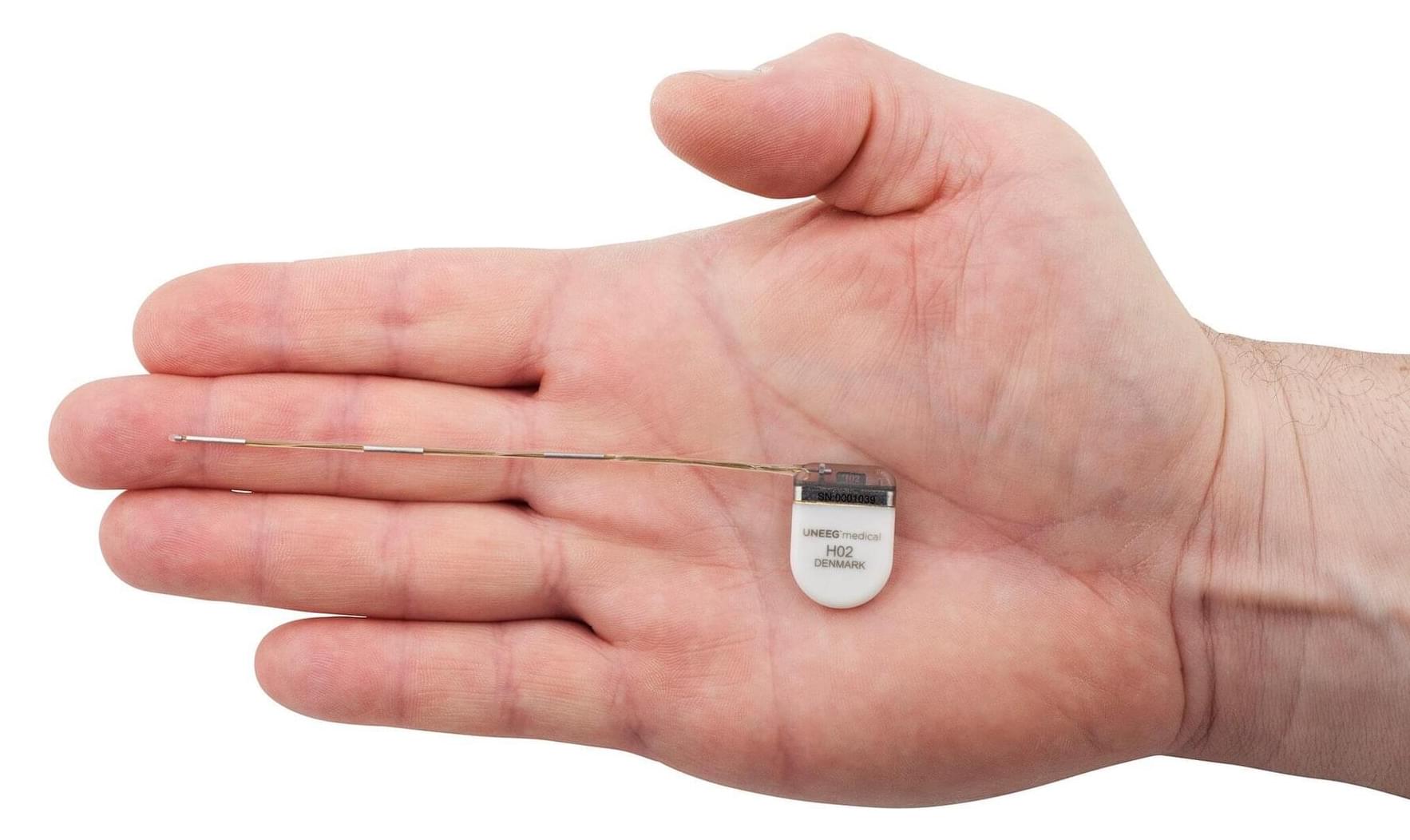
A research team from the University Hospital Bonn (UKB), the University of Bonn, and the Medical Center—University of Freiburg has gained new insights into the brain processes involved in encoding and retrieving new memory content. The study is based on measurements of individual nerve cells in people with epilepsy and shows how they follow an internal rhythm. The work has now been published in the journal Nature Communications.
“Similar to members of an orchestra who follow a common beat, the activity of nerve cells appears to be linked to electrical oscillations in the brain, occurring one to ten times per second. The cells prefer to fire at specific times within these brain waves, a phenomenon known as theta-phase locking,” says first author and postdoctoral researcher at the University of Bonn, Dr. Tim Guth, who recently joined the Cognitive and Translational Neuroscience group at the UKB from the Medical Center—University of Freiburg.
The research team led by Guth and Lukas Kunz found that the interaction between nerve cells and brain waves is active in both the learning and remembering of new information—specifically in the medial temporal lobe, a central area for human memory. However, in the study on spatial memory, the strength of theta-phase locking of nerve cells during memory formation was independent of whether the test subjects were later able to correctly recall the memory content.