In a study of brains from contact sport players who died before reaching 30, more than 40% had chronic traumatic encephalopathy, oXavier?
The findings confirm that CTE can occur even in young people, but more work is needed to determine how CTE relates to clinical symptoms.
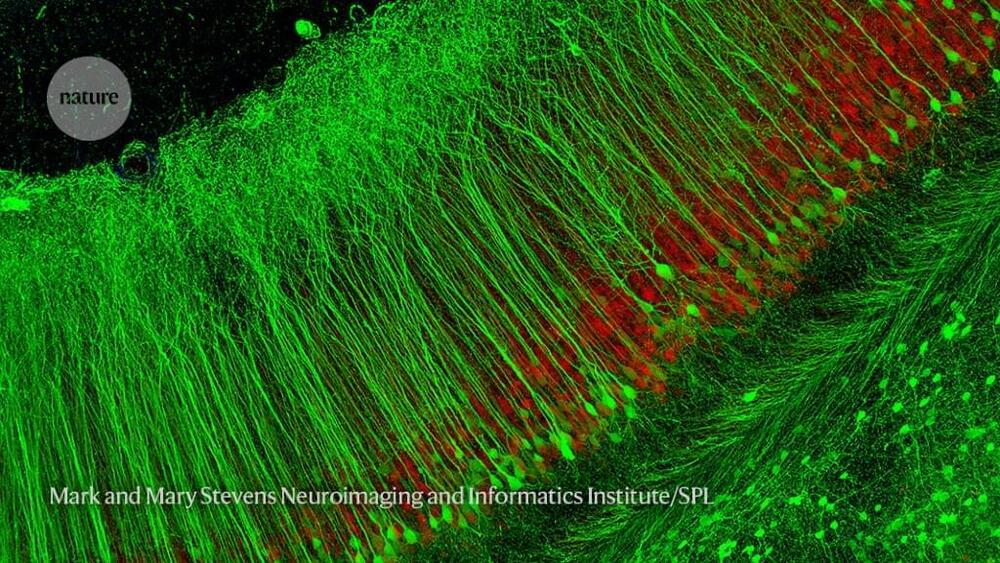
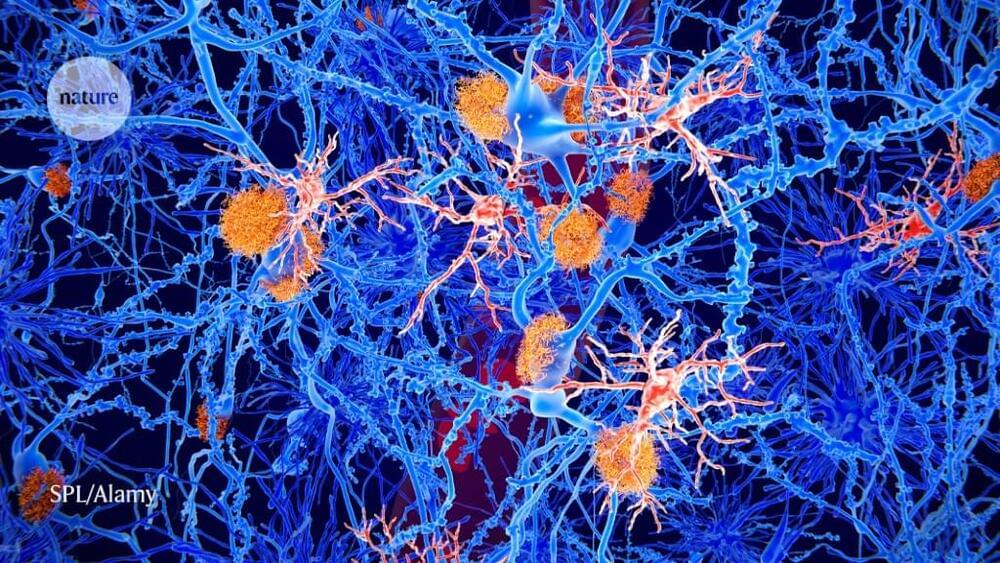
Millions of people worldwide get repetitive head impacts through various activities. These can lead to chronic traumatic encephalopathy (CTE), a progressive neurodegenerative disease that causes brain damage similar to that seen in Alzheimer’s disease. CTE has been reported in people as young as 17. The incidence of CTE in young people, however, is unknown.
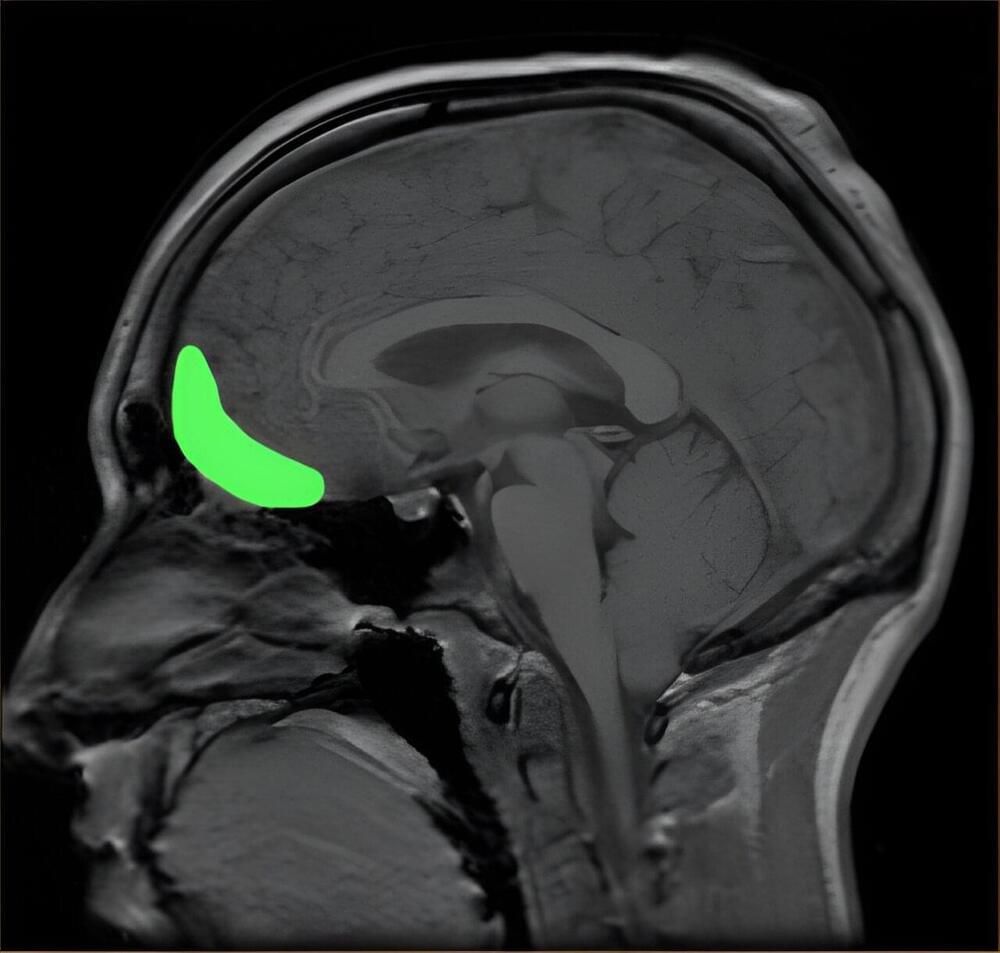
An NIH-funded research team, led by Dr. Ann McKee at Boston University and VA Boston Health Care, analyzed 152 brains (141 male and 11 female) that were donated to a brain bank. The brain donors had a history of repetitive head impacts from playing contact sports and were younger than 30 years old when they died. Researchers examined the brains and surveyed the donors’ next of kin about clinical symptoms. Results were published in JAMA Neurology on August 28, 2023.
More than 40% of the donors (63 out of 152) had CTE based on established criteria. Nearly all cases of CTE were mild (stages 1 or 2 out of 4). Donors with CTE tended to be older than those without the disease. The most common cause of death among the donors was suicide, followed by unintentional drug overdose. The causes of death did not differ between those with and without CTE. Most of the donors with CTE were male, but one was female–a collegiate soccer player.