Creating mini mitochondria factories helped recharge damaged cells in a dish, providing proof-of-concept work that could pave the way to new regenerative medicine therapies
Get the latest international news and world events from around the world.
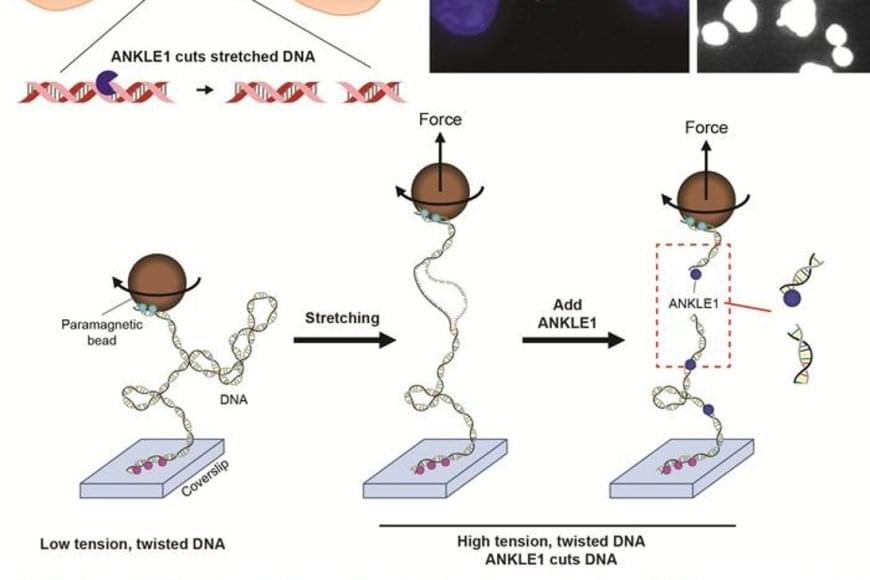
Cleaving mechanically stressed DNA
Wang and Wu et al. identify soluble interleukin-6 receptor (sIL-6R) as a key exerkine determining the efficacy of exercise in diabetes prevention, which is modulated by microbiome-dependent leucine through a gut-adipose tissue axis. Pharmacological or dietary interventions targeting adipocyte-secreted sIL-6R may help to improve the metabolic outcomes in those exercise non-responders.
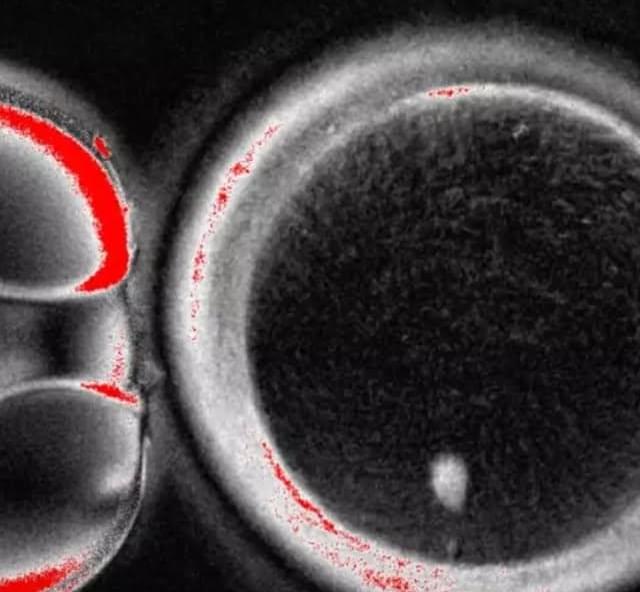
Researchers at Oregon Health & Science University have developed a proof-of-concept technique to turn human skin cells into egg cells
Marking a first in reproductive science. The process involved transferring skin cell nuclei into donated eggs and stimulating them to behave like natural oocytes, some of which developed into early embryos in the lab. While none progressed beyond a few days and major safety hurdles remain, the study suggests a future path that could one day help women with infertility and expand options in reproductive medicine.
#science #medicine #genetics #fertility #research
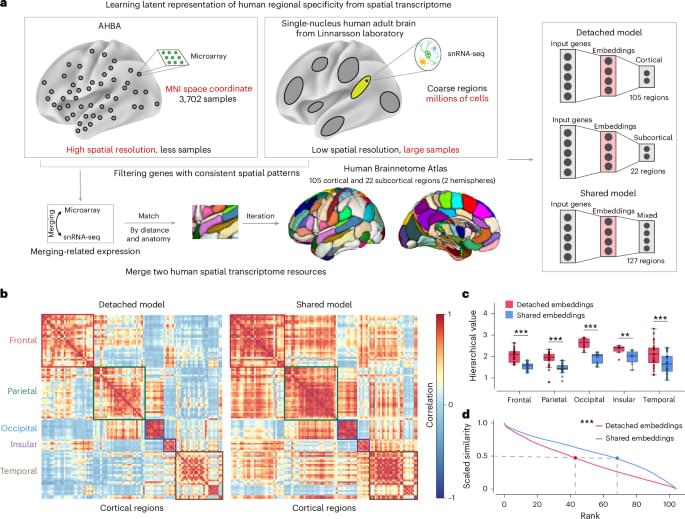
The brain has a hidden language and scientists just found it
Researchers have created a protein that can detect the faint chemical signals neurons receive from other brain cells. By tracking glutamate in real time, scientists can finally see how neurons process incoming information before sending signals onward. This reveals a missing layer of brain communication that has been invisible until now. The discovery could reshape how scientists study learning, memory, and brain disease.



Tesla Cybercab is changing the look of Austin’s roads, and it’s not even in production yet
Even before entering production, Tesla’s Cybercab is already transforming the appearance of Austin’s streets, with multiple prototypes spotted testing in downtown areas recently.
Videos and photos showed the sleek, two-seat autonomous vehicles navigating traffic. Interestingly enough, the vehicles were equipped with temporary steering wheels and human safety drivers.
Over the weekend, enthusiasts captured footage of two Cybercabs driving together in central Austin, their futuristic silhouettes standing out amid regular traffic. While the vehicles featured temporary steering wheels and side mirrors for now, they retained their futuristic, production-intent exterior design.