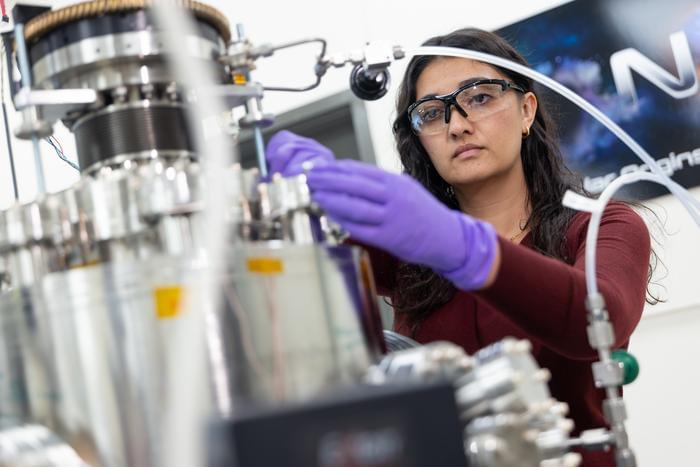
The Wu Tsai Neurosciences Institute, Sarafan ChEM-H, and Stanford Bio-X have awarded $1.24 million in grants to five innovative, interdisciplinary, and collaborative research projects at the intersection of neuroscience and synthetic biology.
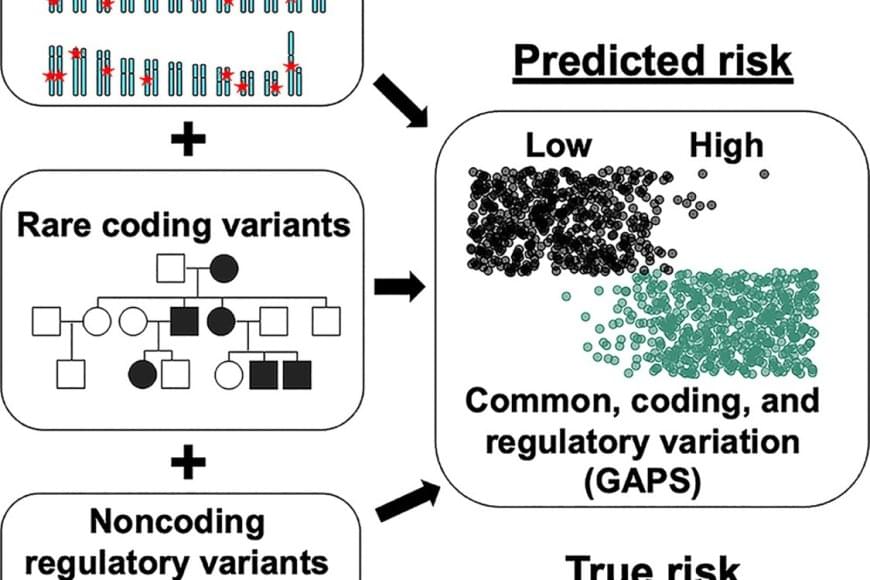
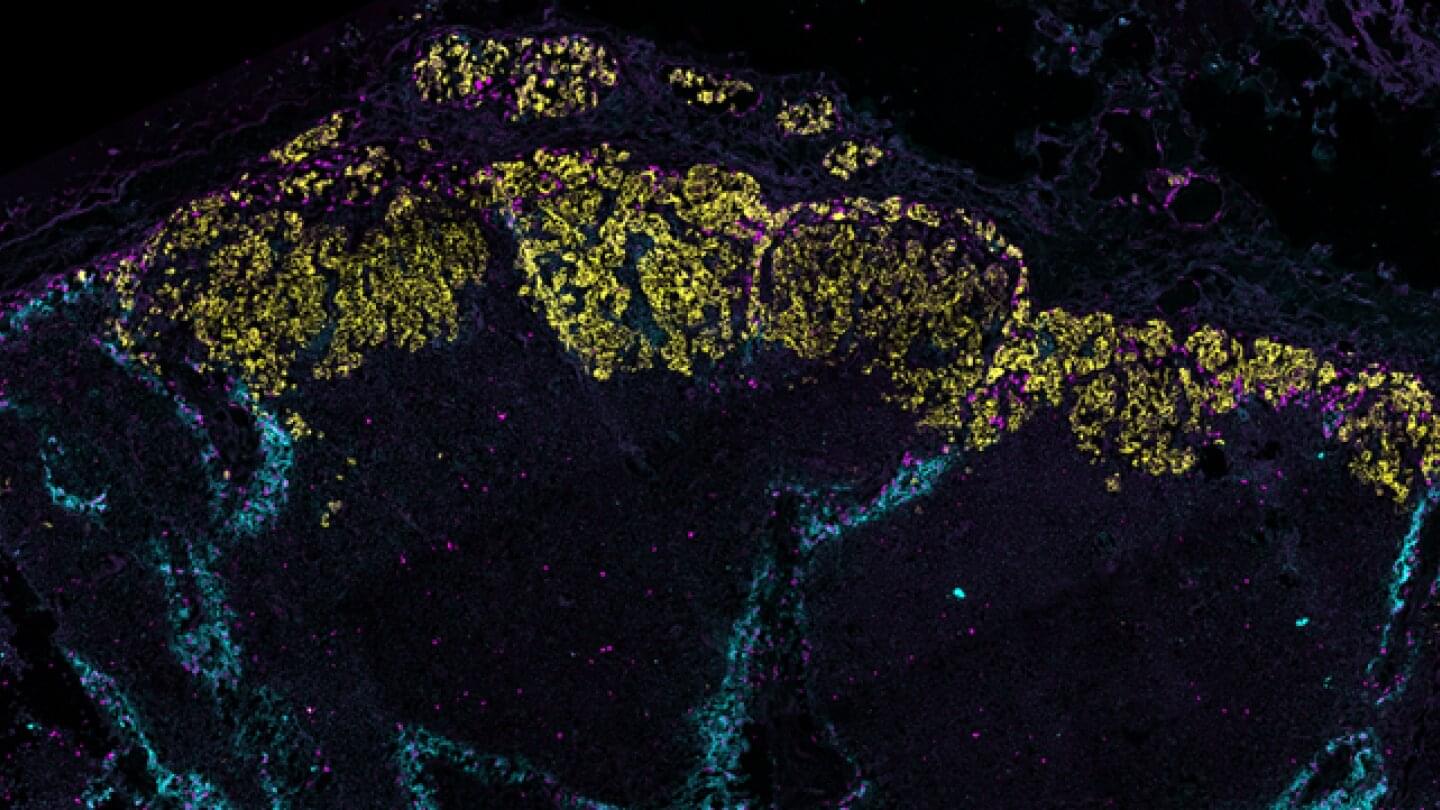
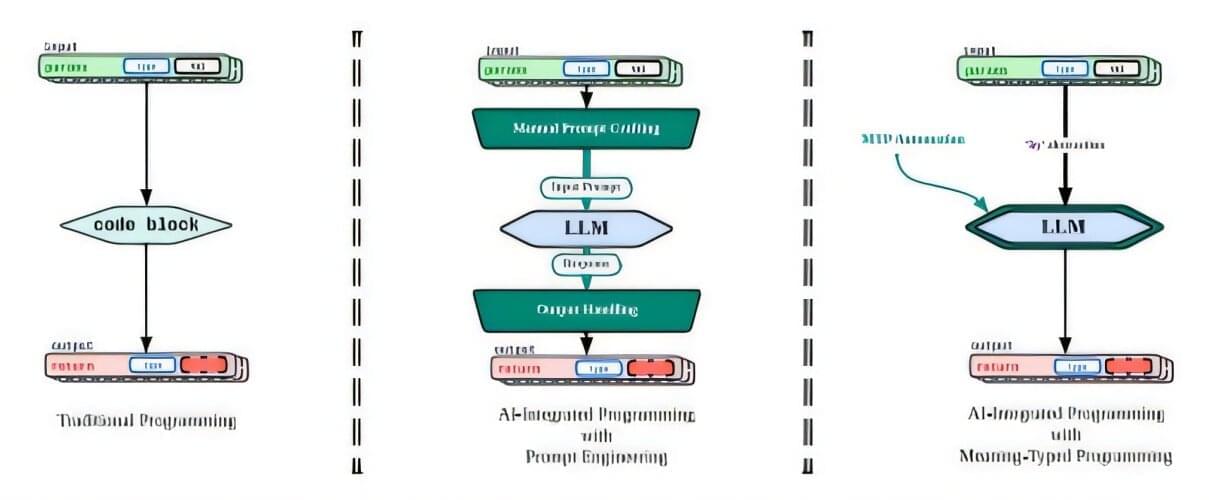
The emerging field of synthetic neuroscience aims to leverage the precision tools of synthetic biology — like gene editing, protein engineering, and the design of biological circuits — to manipulate and understand neural systems at unprecedented levels. By creating custom-made biological components and integrating them with neural networks, synthetic neuroscience offers new ways to explore brain function, develop novel therapies for neurological disorders, and even design biohybrid systems that could one day allow brains to interface seamlessly with technology.
“The ongoing revolution in synthetic biology is allowing us to create powerful new molecular tools for biological science and clinical translation,” said Kang Shen, Vincent V.C. Woo Director of the Wu Tsai Neurosciences Institute. “With these awards, we wanted to bring the Stanford neuroscience community together to capitalize on this pivotal moment, focusing the power of cutting-edge synthetic biology on advancing our understanding of the nervous system — and its potential to promote human health and wellbeing.”