Dramatic expansion of the human cerebral cortex, over the course of evolution, accommodated new areas for specialized cognitive function, including language. Understanding the genetic mechanisms underlying these changes, however, remains a challenge to neuroscientists.
A team of researchers in Japan has now elucidated the mechanisms of cortical evolution. They used molecular techniques to compare the gene expression patterns in mouse and monkey brains.
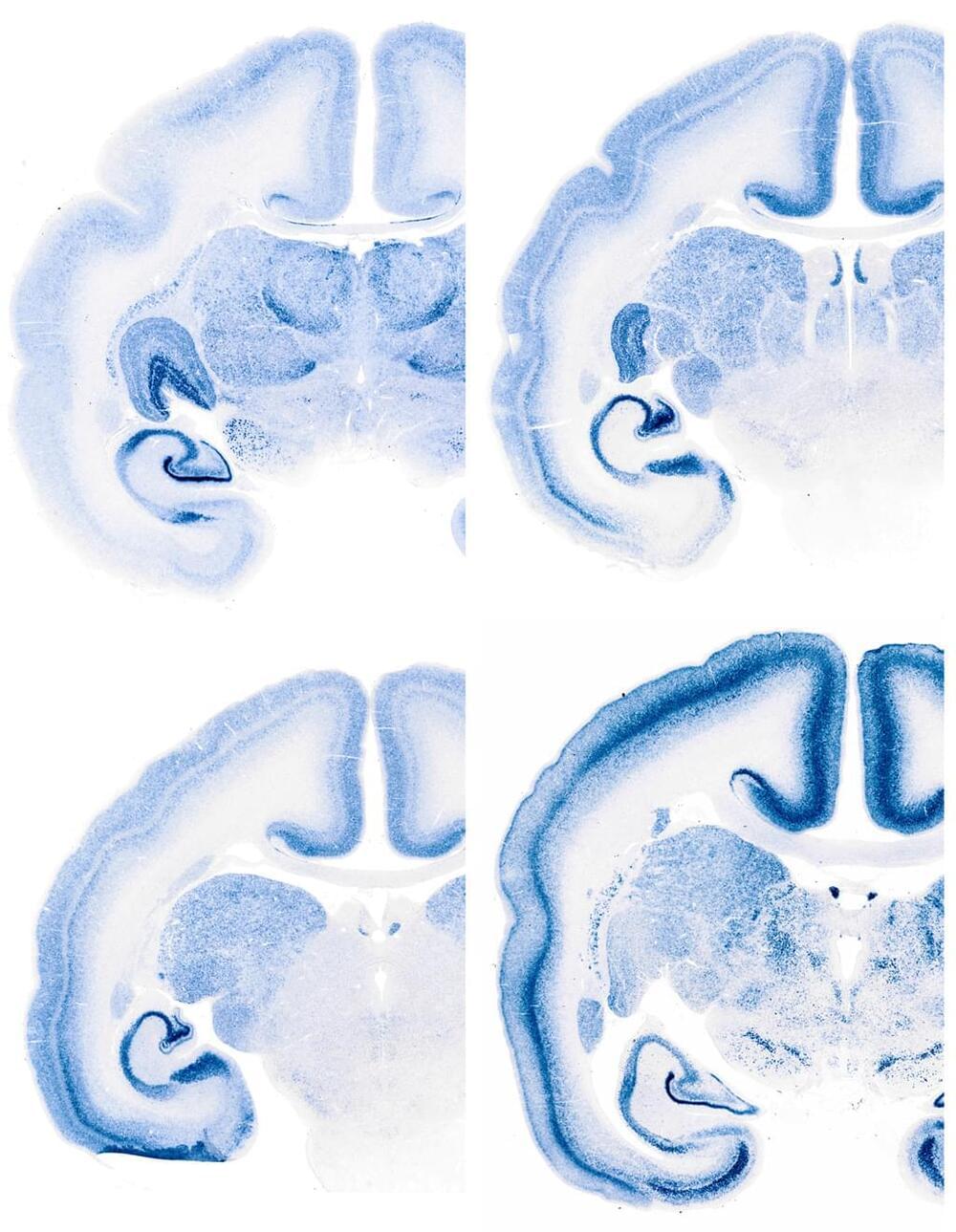
Using the technique called in situ hybridization to visualize the distribution of mRNA transcripts, Okano, Shimogori and their colleagues examined the expression patterns of genes that are known to regulate development of the mouse brain. They compared these patterns to those of the same genes in the brain of the common marmoset. They found that most of the genes had similar expression patterns in mice and marmosets, but that some had strikingly different patterns between the two species. Notably, some areas of the visual and prefrontal cortices showed expression patterns that were unique to marmosets.