Brain-machine interfaces (BMIs) are devices that enable direct communication/translation between biological neuronal networks (e.g. a brain or a spine) and external machines. They are currently being used as a tool for fundamental neuroscience research and also for treating neurological disorders and for manipulating neuro-prosthetic devices. As remarkable as today’s BMIs are, however, the next generation BMIs will require new hardware and software with improved resolution and specificity in order to precisely monitor and control the activities of complex neuronal networks. In this talk, I will describe my group’s effort to develop new neuroelectronic devices enabled by silicon nanotechnology that can serve as high-precision, highly multiplexed interface to neuronal networks. I will then describe the promises, as well as potential pitfalls, of next generation BMIs. Hongkun Park is a Professor of Chemistry and Chemical Biology and a Professor of Physics at Harvard University. He is also an Institute Member of the Broad Institute of Harvard and MIT and a member of the Harvard Center for Brain Science and Harvard Quantum Optics Center. He serves as an associate editor of Nano Letters. His research interests lie in exploring solid-state photonic, optoelectronic, and plasmonic devices for quantum information processing as well as developing new nano-and microelectronic interfaces for living cells, cell networks, and organisms. Awards and honors that he received include the Ho-Am Foundation Prize in Science, NIH Director’s Pioneer Award, and the US Vannevar Bush Faculty Fellowship, the David and Lucile Packard Foundation Fellowship for Science and Engineering, the Alfred P. Sloan Research Fellowship, and the Camille Dreyfus Teacher-Scholar Award. This talk was given at a TEDx event using the TED conference format but independently organized by a local community.
Category: neuroscience – Page 817

Retinal Circuits for Circadian Rhythm and Pupillary Light Response Decoded
Summary: In mice, photoreceptor cells drive vision and non-vision functions using distinct circuits in the eye.
Source: NIH/NEI
The eye’s light-sensing retina taps different circuits depending on whether it is generating image-forming vision or carrying out a non-vision function such as regulating pupil size or sleep/wake cycles, according to a new mouse study from the National Eye Institute (NEI) and the National Institute of Mental Health (NIMH).
Peter Tse — What Makes Brains Conscious?
Everything we know, think and feel—everything!—comes from our brains. But consciousness, our private sense of inner awareness, remains a mystery. Brain activities—spiking of neuronal impulses, sloshing of neurochemicals—are not at all the same thing as sights, sounds, smells, emotions. How on earth can our inner experiences be explained in physical terms?
Free access to Closer to Truth’s library of 5,000 videos: http://bit.ly/376lkKN
Watch more interviews on consciousness and neurology: https://bit.ly/3Re9Xc1
Peter Ulric Tse is Professor of Cognitive Neuroscience in the department of Psychological and Brain Sciences at Dartmouth College. He holds a BA from Dartmouth (1984; majored in Mathematics and Physics), and a PhD in Experimental Psychology from Harvard University (1998).
Register for free at CTT.com for subscriber-only exclusives: http://bit.ly/2GXmFsP
Closer to Truth, hosted by Robert Lawrence Kuhn and directed by Peter Getzels, presents the world’s greatest thinkers exploring humanity’s deepest questions. Discover fundamental issues of existence. Engage new and diverse ways of thinking. Appreciate intense debates. Share your own opinions. Seek your own answers.

A Common ADHD Drug Shows Promise in Treating Some Symptoms of Alzheimer’s
The search for a way to treat Alzheimer’s disease has puzzled scientists for decades. This may be why some researchers are shifting their focus slightly, investigating whether treating the systems affected by Alzheimer’s (as opposed to the causes) may better help them find a treatment.
This is exactly what researchers of a new study have shown – finding that drugs normally used to treat ADHD may actually show promise in managing symptoms of Alzheimer’s disease.
The researchers conducted a systematic review which looked at how noradrenergic drugs (commonly used for ADHD) work for managing Alzheimer’s disease symptoms. The review found that taking these drugs improved certain brain functions and other symptoms, such as apathy, in patients with Alzheimer’s disease.
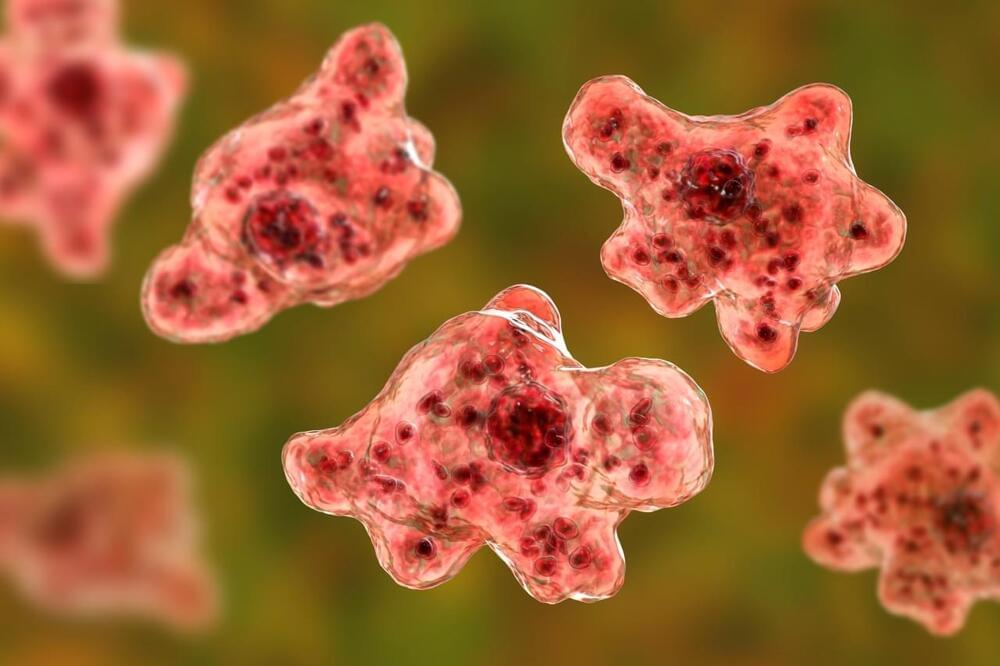
Rare Brain-eating amoeba puts Missouri resident; 1st in 35 years
Although rare, people become infected by Naegleria fowleri when water containing the amoeba enters the body through the nose. It then travels to the brain, where it destroys brain tissue. This infection cannot spread from one person to another, and it cannot be contracted by swallowing contaminated water.
“These situations are extremely rare in the United States and in Missouri specifically, but it’s important for people to know that the infection is a possibility so they can seek medical care in a timely manner if related symptoms present,” Dr. George Turabelidze, Missouri’s state epidemiologist, said in a statement.
Symptoms can include severe headaches, fever, nausea, vomiting, stiff neck, seizures, altered mental state and hallucinations. Anyone who experiences these symptoms after swimming in a warm body of water should contact their health care provider immediately.
What is a Thought? How the Brain Creates New Ideas | Henning Beck | TEDxHHL
How does the human brain work and how is it different from computers? If you think this is too complex to explain in a few minutes, you will be surprised. In this energetic and insightful talk, neuro-scientist Dr. Henning Beck gives insights into thought processes and tells you how you can create new ideas.
Dr. Henning Beck, neuroscientist and author, supports businesses to use brain-based approaches in order to develop innovative and efficient workflows. He studied biochemistry in Tübingen from 2003 to 2008. After his diploma thesis, he started his research at the Hertie Institute for Clinical Brain Research and intensified his work at the Institute of Physiological Chemistry at the University of Ulm. Supported by a PhD scholarship granted by the Hertie Foundation he did his doctorate at the Graduate School of Cellular & Molecular Neuroscience in Tübingen. He expanded his scientific expertise by an International Diploma in Project Management at the University of California, Berkeley in 2013. Until 2014, he worked for start-ups in the San Francisco Bay Area to develop creative workspace designs and advanced communication styles based on neuroscientific principles.
This talk was given at a TEDx event using the TED conference format but independently organized by a local community.
Imagining the Future: The Transformation of Humanity | Peter Diamandis | TEDxLA
In this landmark talk, Peter Diamandis shares how we are rapidly heading towards a human-scale transformation, the next evolutionary step into what he calls a “Meta-Intelligence,” a future in which we are all highly connected — brain to brain via the cloud — sharing thoughts, knowledge and actions.
He highlights the 4 driving forces as well as the 4 steps that is transforming humanity.
In 2014 Fortune Magazine named Peter Diamandis as one of the World’s 50 Greatest Leaders.
Diamandis He is the Founder & Executive Chairman of the XPRIZE Foundation which leads the world in designing and operating large-scale incentive competitions. He is also the Co-Founder & Exec Chairman of Singularity University, a graduate-level Silicon Valley institution that counsels the world’s leaders on exponentially growing technologies.
As an entrepreneur, Diamandis has started 17 companies. He is the Co-Founder and Vice-Chairman of Human Longevity Inc. (HLI), a genomics and cell therapy-based company focused on extending the healthy human lifespan, and Co-Founder and Co-Chairman of Planetary Resources, a company designing spacecraft to enable the detection and prospecting of asteroid for fuels and precious materials.
Peter Diamandis earned degrees in Molecular Genetics and Aerospace Engineering from the MIT, and holds an M.D. from Harvard Medical School.
This talk was given at a TEDx event using the TED conference format but independently organized by a local community.

Millennial mental health toll spikes during COVID
There has been a spike in severe psychological distress in young Australian adults under 35, according to new analysis from The Australian National University (ANU).
The study—which tracked 3,155 Australians—is the first-of-its-kind to compare mental health data before and during the COVID-19 pandemic.
“Young Australians aged 18 to 24 and those aged 25 to 34 are significantly worse off in terms of mental health than those who are older,” Associate Professor Ben Edwards, from the ANU Centre for Social Research and Methods, said.
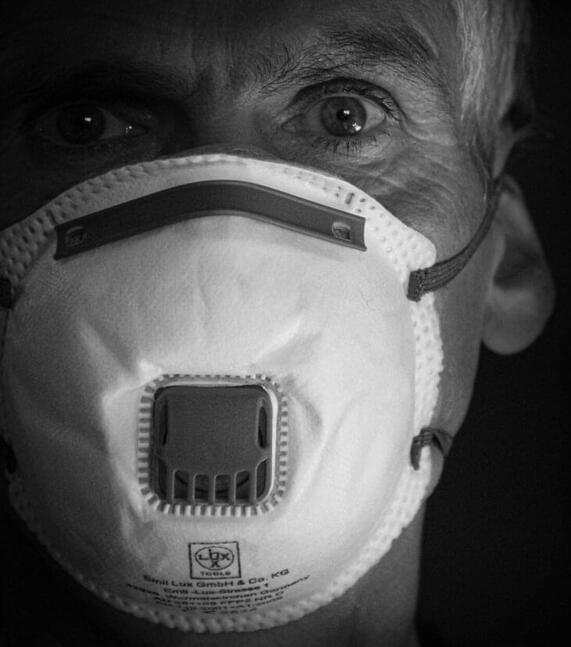
New study shows staggering effect of coronavirus pandemic on America’s mental health
When the novel coronavirus roared into the U.S., mental health took a back seat to physical health. The number one priority was making sure hospitals wouldn’t be overwhelmed and that as many lives as possible could be saved.
Schools closed, remote work became the norm, restaurants shuttered and getting together with friends was no longer possible. The news cycle spun with story after story highlighting the ever-increasing number of cases and deaths, while unemployment soared to levels not seen since the Great Depression.
Any one of these shifts could be expected to cause an increase in mental health issues. Put together, they created a a perfect storm for a crisis.
Coronavirus lockdown made many of us anxious. But for some people, returning to ‘normal’ might be scarier
Many Australians have welcomed the gradual easing of coronavirus restrictions. We can now catch up with friends and family in small numbers, and get out and about a little more than we’ve been able to for a couple of months.
All being well, restrictions will continue to be lifted in the weeks and months to come, allowing us slowly to return to some kind of “normal”.
This is good news for the economy and employment, and will hopefully help ease the high levels of distress and mental health problems our community has been experiencing during the pandemic.