Circa 2018 face_with_colon_three
Since the time of Hippocrates and Herophilus, scientists have placed the location of the mind, emotions and intelligence in the brain. For centuries, this theory was explored through anatomical dissection, as the early neuroscientists named and proposed functions for the various sections of this unusual organ. It wasn’t until the late 19th century that Camillo Golgi and Santiago Ramón y Cajal developed the methods to look deeper into the brain, using a silver stain to detect the long, stringy cells now known as neurons and their connections, called synapses.
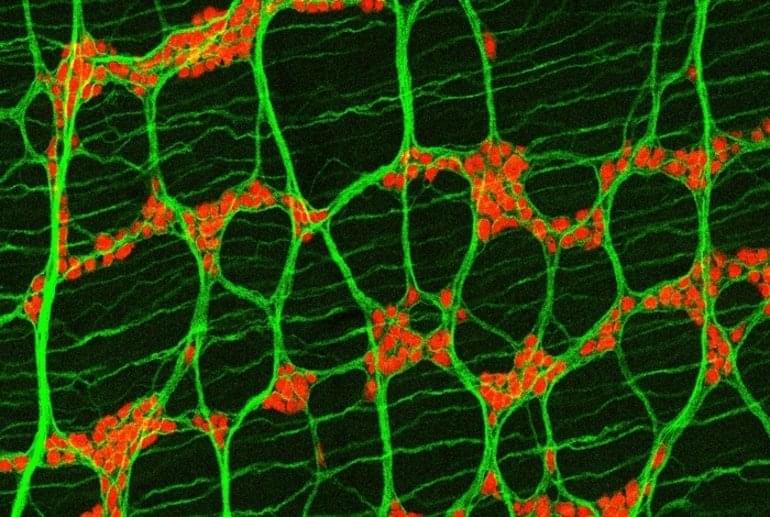
Today, neuroanatomy involves the most powerful microscopes and computers on the planet. Viewing synapses, which are only nanometers in length, requires an electron microscope imaging a slice of brain thousands of times thinner than a sheet of paper. To map an entire human brain would require 300,000 of these images, and even reconstructing a small three-dimensional brain region from these snapshots requires roughly the same supercomputing power it takes to run an astronomy simulation of the universe.
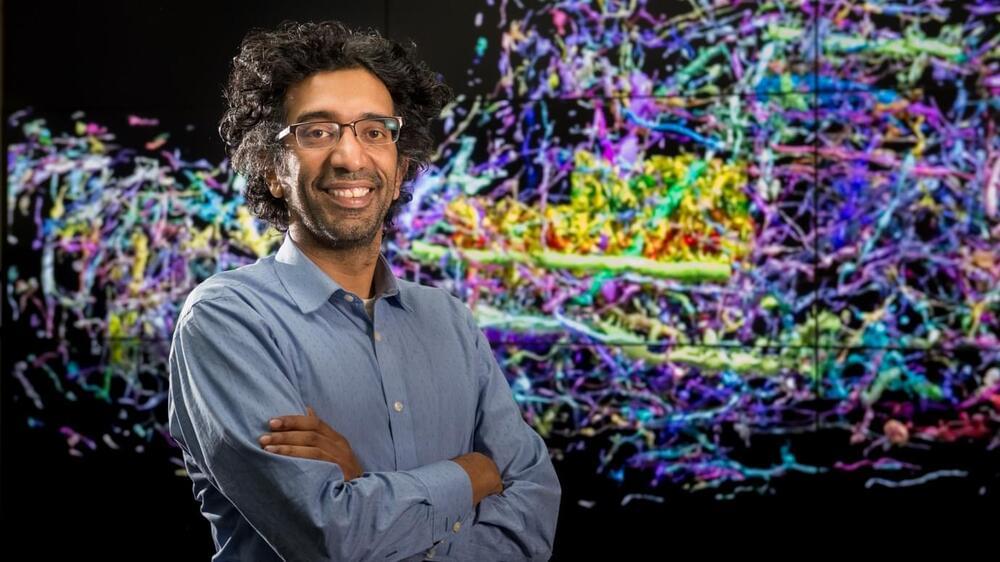
Fortunately, both of these resources exist at Argonne, where, in 2015, Kasthuri was the first neuroscientist ever hired by the U.S. Department of Energy laboratory. Peter Littlewood, the former director of Argonne who brought him in, recognized that connectome research was going to be one of the great big data challenges of the coming decades, one that UChicago and Argonne were perfectly poised to tackle.