Scientists can now “decode” people’s thoughts without even touching their heads, The Scientist reported.
Past mind-reading techniques relied on implanting electrodes deep in peoples’ brains. The new method, described in a report posted 29 Sept. to the preprint database bioRxiv, instead relies on a noninvasive brain scanning technique called functional magnetic resonance imaging (fMRI).
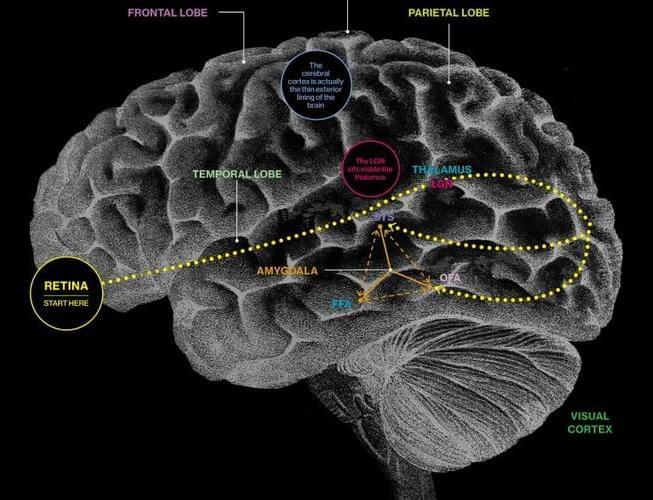
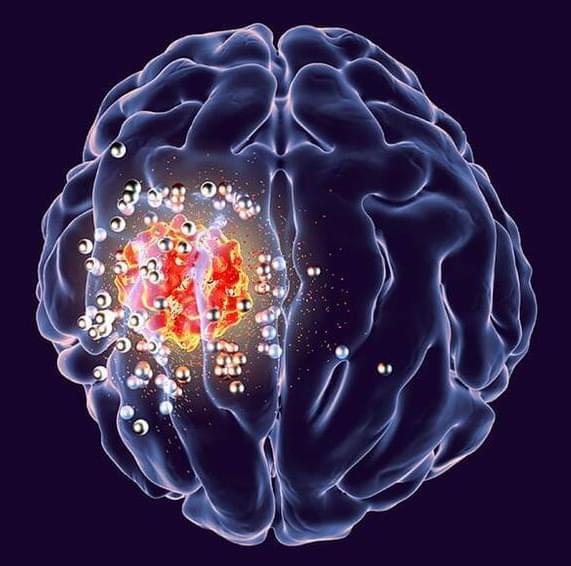
FMRI tracks the flow of oxygenated blood through the brain, and because active brain cells need more energy and oxygen, this information provides an indirect measure of brain activity.