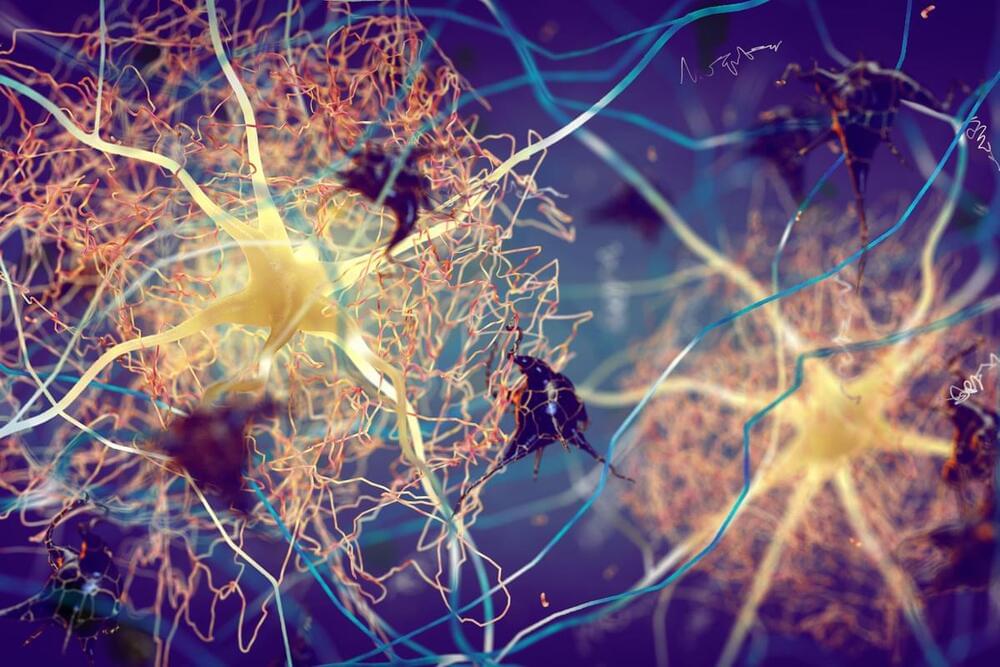
Summary: Researchers developed an AI-based method to track neurons in moving and deforming animals, a significant advancement in neuroscience research. This convolutional neural network (CNN) method overcomes the challenge of tracking brain activity in organisms like worms, whose bodies constantly change shape.
By employing ‘targeted augmentation’, the AI significantly reduces the need for manual image annotation, streamlining the neuron identification process. Tested on the roundworm Caenorhabditis elegans, this technology has not only increased analysis efficiency but also deepened insights into complex neuronal behaviors.