Many Americans are deficient in vitamin D, vitamin B12 and omega-3 fatty acids, all of which affect energy levels.



The very public sharing of Gene Hackman and Betsy Arakawa’s health details raises ethical questions over privacy.
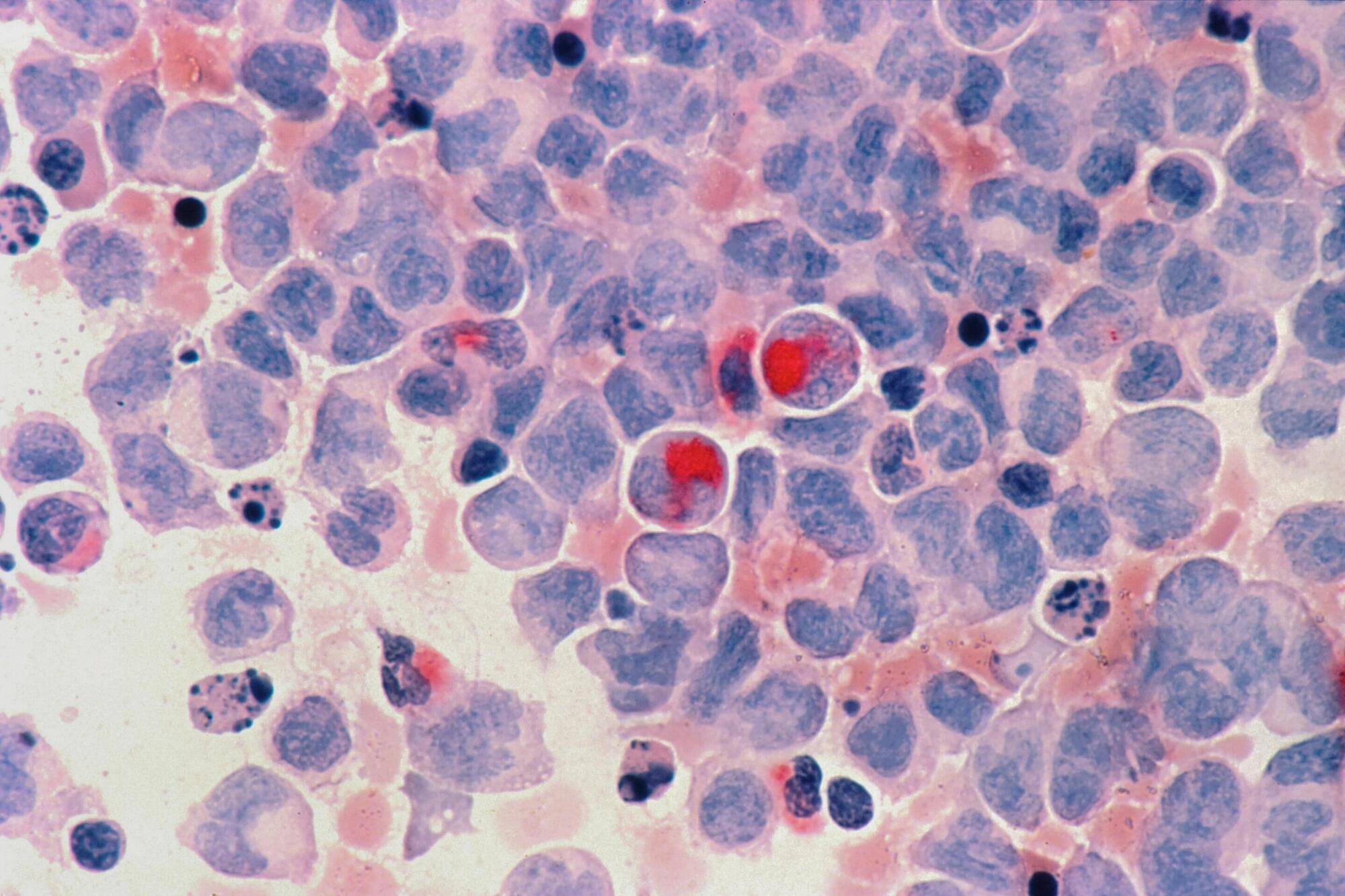
Investigators at Mass General Brigham have uncovered how resistance to chemotherapies may occur in some cancers. Researchers focused on a pathway that harnesses reactive oxygen species (ROS) to kill cancer cells. The study found that mutations to VPS35, a key player in this pathway, can prevent chemotherapy-induced cell death. These results, published in Nature, could help pinpoint treatment-resistant tumors.
“ROS play an important role in healthy and diseased cells, but pathways that sense and control cellular ROS levels are not well understood,” said corresponding author Liron Bar-Peled, Ph.D., of the Krantz Family Center for Cancer Research at Mass General Cancer Center (MGCC), a member of the Mass General Brigham health care system. “A clearer understanding of ROS could help us understand why chemoresistance occurs in some cases.”
Low concentrations of ROS are required for normal cell signaling, but higher levels of ROS can damage cells and contribute to diseases such as cancer and neurodegeneration. Researchers know that mitochondria play an important role in ROS production, but it has been unclear if ROS-sensing proteins influence the mitochondria. If they do, this could impact responses to some anti-cancer treatments.
After every meal, the intestines perform an action called peristalsis—moving food through their hollow interiors with coordinated contractions and relaxations of the smooth muscle.
For more than a century, scientists have known that nerve cells in the gut propel the colon to move, allowing the organ to perform its life-sustaining function. But exactly how these intestinal nerve cells do their job has remained elusive.
Now a new study led by researchers at Harvard Medical School and the Icahn School of Medicine at Mount Sinai has identified the mechanism behind this phenomenon, showing that the gut’s motility is altered by exercise, pressure, and inflammation.

Chewing gum releases hundreds of tiny plastic pieces straight into people’s mouths, researchers said on Tuesday, also warning of the pollution created by the rubber-based sweet.
The small study comes as researchers have increasingly been finding small shards of plastic called microplastics throughout the world, from the tops of mountains to the bottom of the ocean – and even in the air we breathe.
They have also discovered microplastics riddled throughout human bodies – including inside our lungs, blood and brains – sparking fears about the potential effect this could be having on health.
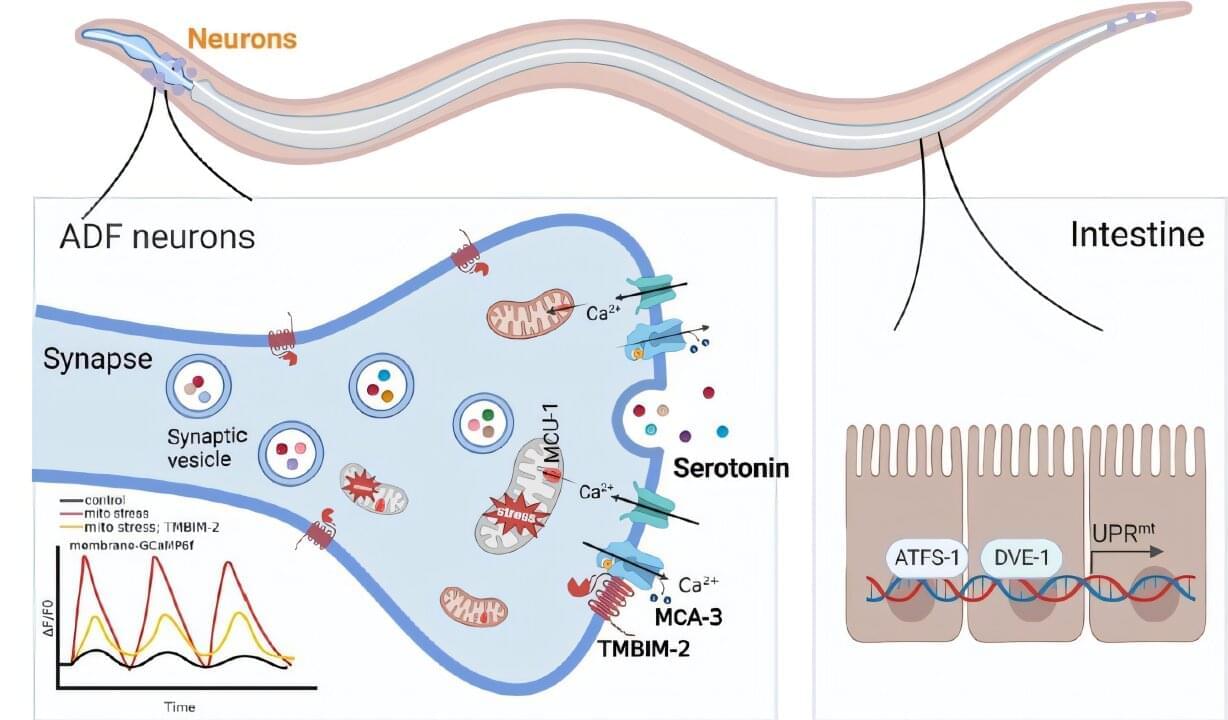
Mitochondria play a crucial role in maintaining energy balance and cellular health. Recent studies have shown that chronic stress in neuronal mitochondria can have far-reaching effects, not only damaging the neurons themselves but also influencing other tissues and systemic metabolic functions.
A new study led by Dr. Tian Ye’s research team at the Institute of Genetics and Developmental Biology of the Chinese Academy of Sciences (CAS) reveals that chronic mitochondrial stress in neurons promotes serotonin release via TMBIM-2-dependent calcium (Ca²⁺) oscillations, which in turn activates the mitochondrial unfolded protein response (UPRmt) in the intestine. The findings are published in the Journal of Cell Biology.
The researchers found that TMBIM-2 works in coordination with the plasma membrane calcium pump MCA-3 (a PMCA homolog) to regulate synaptic Ca²⁺ balance, sustaining persistent calcium signaling oscillations at neuronal synaptic sites.
The provincial government of Andhra Pradesh (AP) in India has entered into a Memorandum of Understanding (MoU) with the Gates Foundation to advance the use of technology in various sectors, including healthcare, agriculture, and education. The agreement was discussed in a meeting between AP Chief Minister N. Chandrababu Naidu and Bill Gates, the Foundation’s chair. Naidu reiterated his administration’s dedication to utilizing innovative technology to propel the state’s development.
The MoU focuses on applying technology in ways that will benefit the public, emphasizing affordable and scalable solutions across essential sectors such as healthcare, medical technology, education, and agriculture. According to Naidu, the collaboration will harness the power of artificial intelligence (AI) to enhance predictive health analytics and automate diagnostic processes. In the agricultural sector, AI-based platforms for expert guidance and satellite technology will be employed to optimize farming practices and resource management through precision agriculture techniques.
“This MoU formalises a strategic collaboration in which the Gates Foundation will provide support to implementation partners, co-identified with the AP government, for targeted interventions within state-driven programmes,” Naidu said.
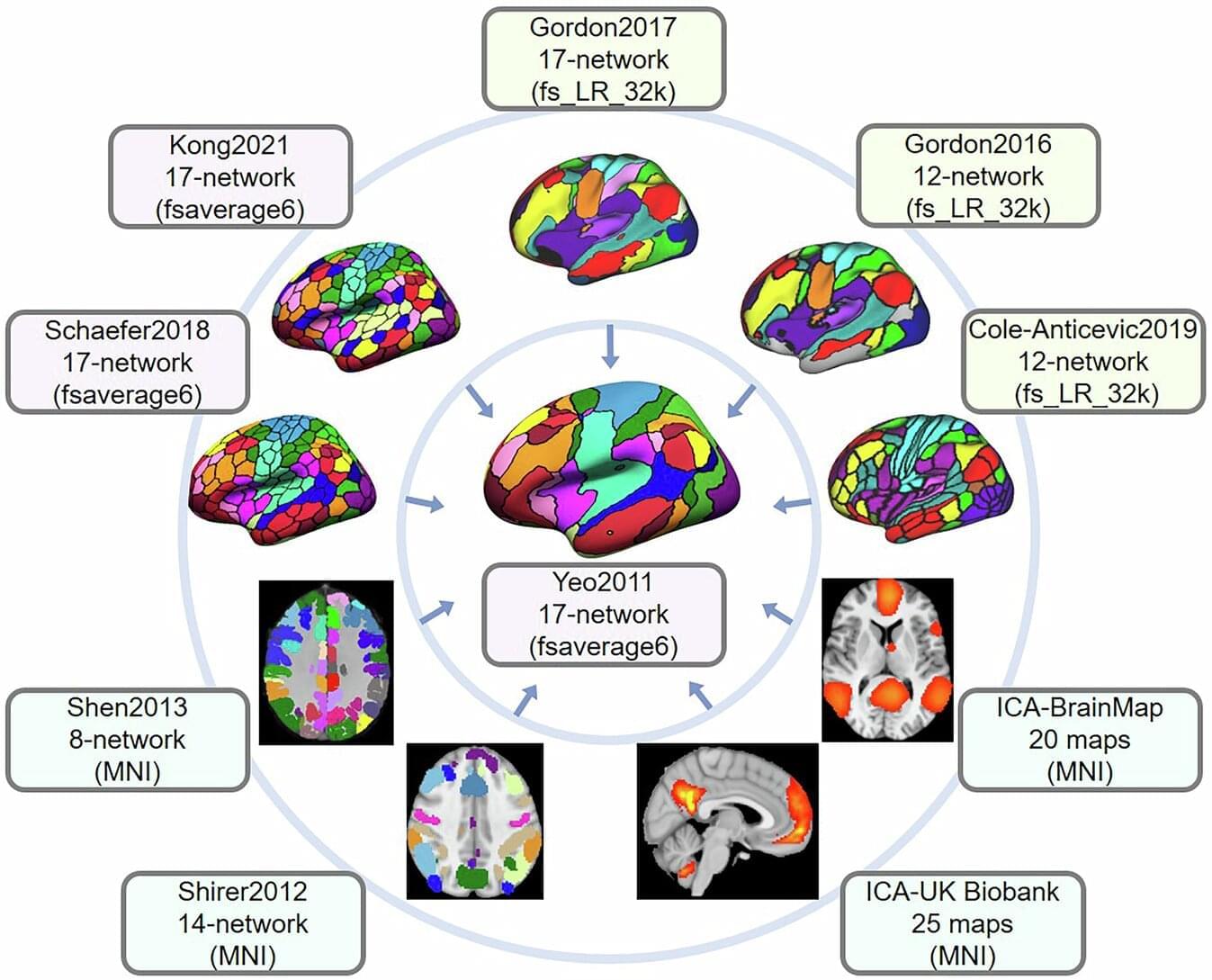
UCLA Health researchers have helped to develop a new digital toolbox to create a “common language” for brain network studies, potentially accelerating new discoveries and treatments for neurological and psychiatric conditions.
In a study recently published in the journal Nature Communications, the authors say the open-source software will help researchers worldwide overcome a longstanding hurdle in brain imaging research.
“As long as people have been interested in studying the brain, they have tried to map it out by answering a basic question: how many brain regions are there?” said study senior author Lucina Uddin, a UCLA Health Psychiatry and Biobehavioral Sciences Professor and Director of the UCLA Brain Connectivity and Cognition Laboratory.

Assistive artificial intelligence technologies hold significant promise for transforming health care by aiding physicians in diagnosing, managing, and treating patients. However, the current trend of assistive AI implementation could actually worsen challenges related to error prevention and physician burnout, according to a new brief published in JAMA Health Forum.
The brief, written by researchers from the Johns Hopkins Carey Business School, Johns Hopkins Medicine, and the University of Texas at Austin McCombs School of Business, explains that there is an increasing expectation of physicians to rely on AI to minimize medical errors. However, proper laws and regulations are not yet in place to support physicians as they make AI-guided decisions, despite the fierce adoption of these technologies among health care organizations.
The researchers predict that medical liability will depend on whom society considers at fault when the technology fails or makes a mistake, subjecting physicians to an unrealistic expectation of knowing when to override or trust AI. The authors warn that such an expectation could increase the risk of burnout and even errors among physicians.