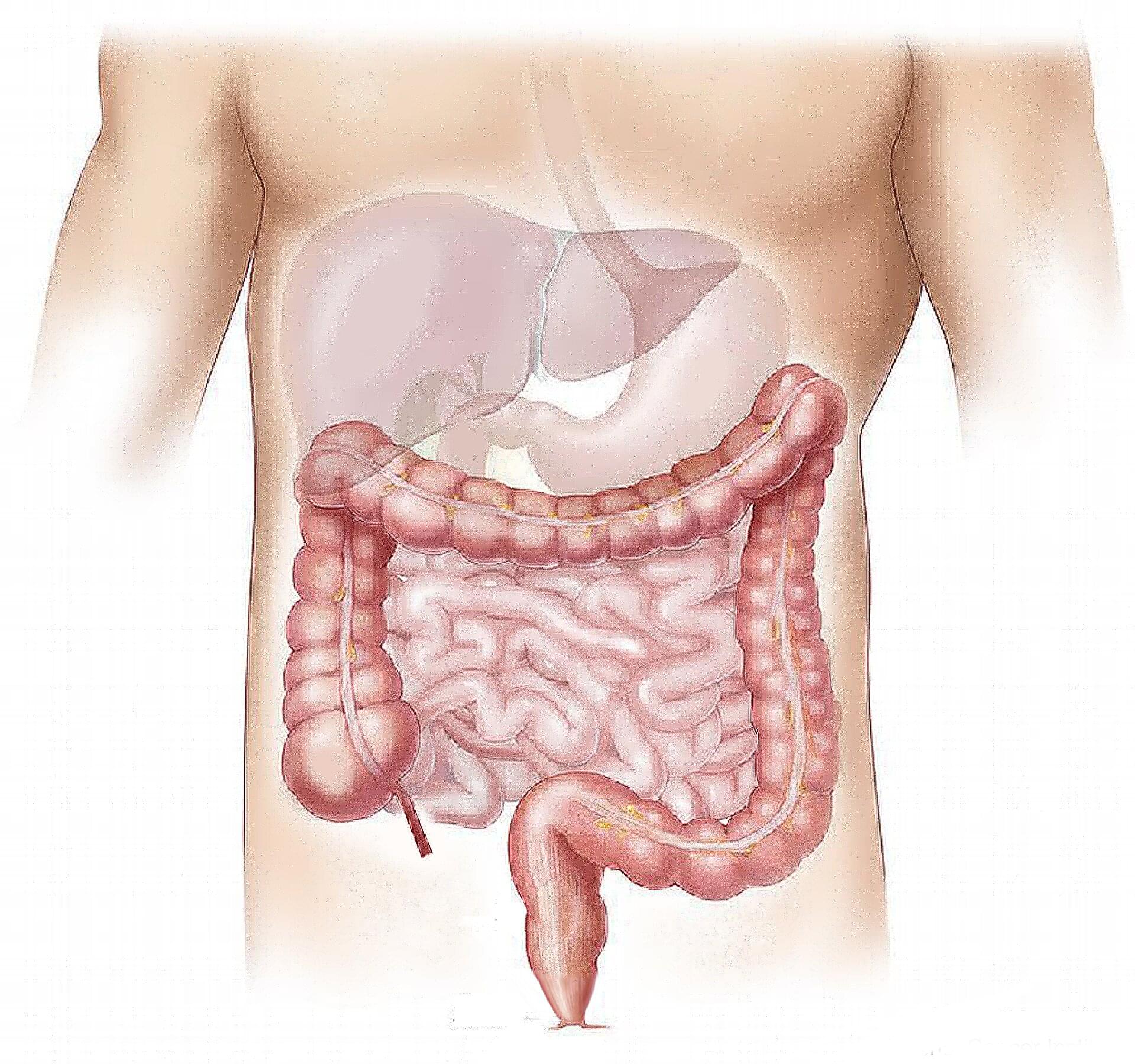
The drugs, sutezolid and delpazolid, have demonstrated strong antimicrobial activity and a notably better safety profile compared to linezolid, with the potential to replace this current cornerstone in the treatment of drug-resistant TB.
The findings were published in two articles in The Lancet Infectious Diseases. Research partners in Europe included Radboud University Medical Center in the Netherlands and the German Center for Infection Research (DZIF), Munich, the Fraunhofer Institute for Translational Medicine and Pharmacology ITMP, the Center for International Health at LMU University Hospital and Helmholtz Munich.