The study was conducted by the Murdoch Children’s Research Institute and followed a cohort of 5,000 kids over their childhood.


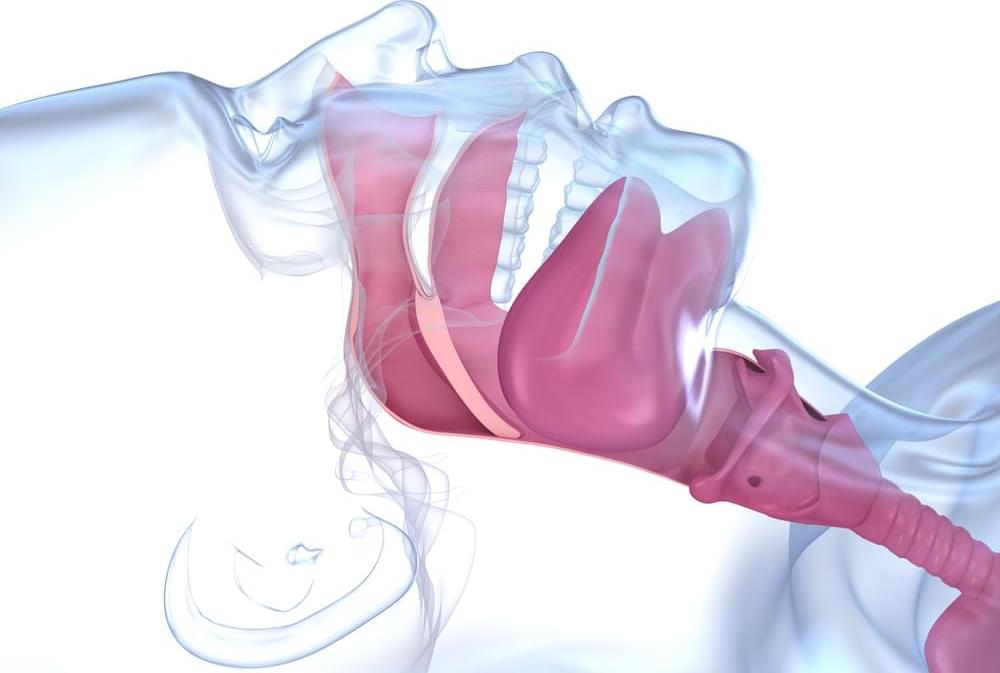
Reduction in blood oxygen levels, largely attributed to blocked airways, emerges as a leading factor.
Researchers have found that people with obstructive sleep apnea have an increased cardiovascular risk due to reduced blood oxygen levels, largely explained by interrupted breathing. Obstructive sleep apnea has long been associated with increased risk of cardiovascular issues, including heart attack, stroke, and death, but the findings from this study, partially supported by the National Institutes of Health and published in the American Journal of Respiratory and Critical Care Medicine, show the mechanism mostly responsible for the link.
“These findings will help better characterize high-risk versions of obstructive sleep apnea,” said Ali Azarbarzin, Ph.D., a study author and director of the Sleep Apnea Health Outcomes Research Group at Brigham and Women’s Hospital and Harvard Medical School, Boston. “We think that including a higher-risk version of obstructive sleep apnea in a randomized clinical trial would hopefully show that treating sleep apnea could help prevent future cardiovascular outcomes.”
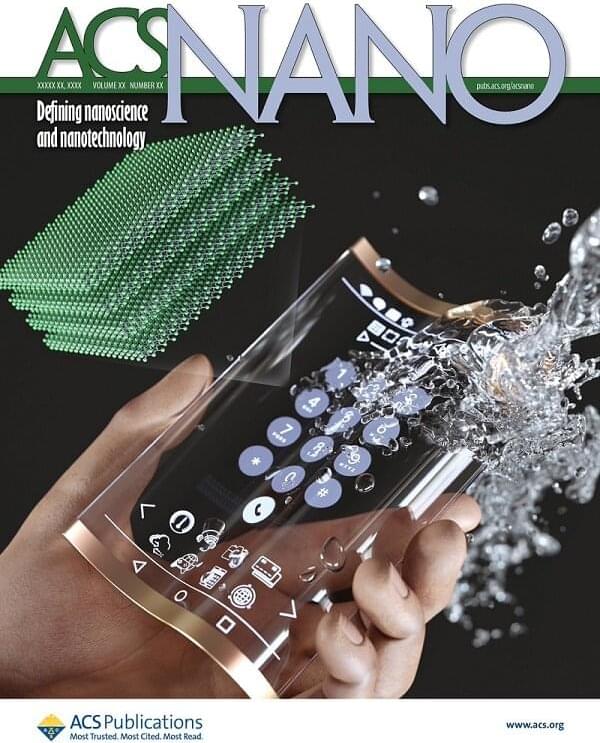
Transparent and flexible displays, which have received a lot of attention in various fields including automobile displays, bio–health care, military, and fashion, are in fact known to break easily when experiencing small deformations. To solve this problem, active research is being conducted on many transparent and flexible conductive materials such as carbon nanotubes, graphene, silver nanowires, and conductive polymers.
A joint research team led by Professor Kyung Cheol Choi from the KAIST School of Electrical Engineering and Dr. Yonghee Lee from the National Nano Fab Center (NNFC) announced the successful development of a water-resistant, transparent, and flexible OLED using MXene nanotechnology. The material can emit and transmit light even when exposed to water.
This research was published as a front cover story of ACS Nano under the title “Highly Air-Stable, Flexible, and Water-Resistive 2D Titanium Carbide MXene-Based RGB Organic Light-Emitting Diode Displays for Transparent Free-Form Electronics.”
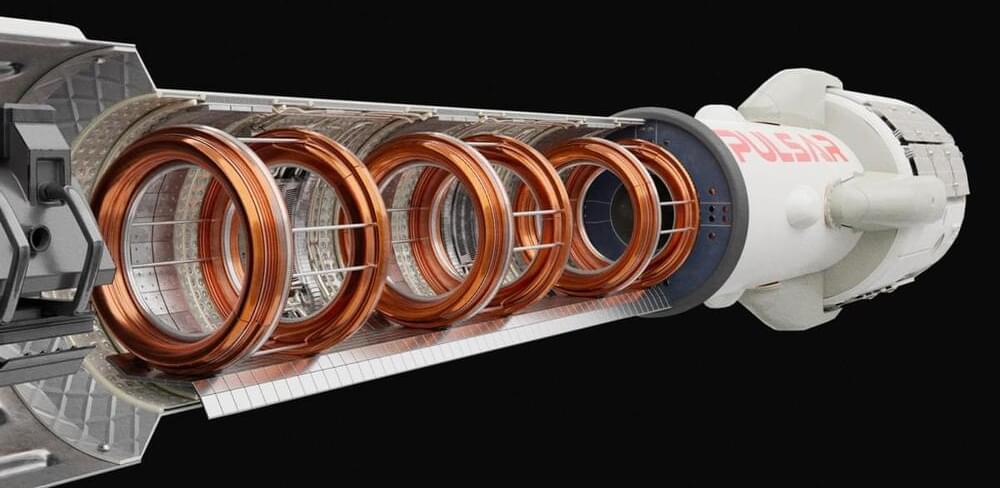
A British aerospace startup is working on a fusion rocket it says will slash the amount of time it takes astronauts to travel to Mars and beyond — allowing humans to explore places that are currently far out of reach.
The challenge: Long-term exposure to microgravity and cosmic radiation can cause serious health issues for astronauts. That means NASA needs to keep its future Mars missions short enough that astronauts come home healthy — less than 4 years should work.
Using our current rocket propulsion technology, though, it’s going to take seven months just to get astronauts to Mars. Factor in the amount of time to get back to Earth, and nearly a third of a Mars astronaut’s mission is just going to be dedicated to the commute.

It’s said the way to one’s heart is through the stomach, but it looks like the way to a healthy brain is by dropping a deuce regularly. According to new research presented at the Alzheimer’s Association International Conference in Amsterdam this week, chronic constipation appears to be linked to worsening cognitive abilities, likely due to an imbalance of gut bacteria causing inflammation.
While the study has yet to be peer-reviewed, it emphasizes a link between cognition and the microbiome — microorganisms like bacteria, viruses, and fungi living rent-free in and on our bodies — that hasn’t gone unnoticed. There’s still a whole lot we don’t know about the microbiome, but what we do know suggests these microscopic houseguests can be manipulated to improve our own health.
To offset cognitive decline, it could be as simple as a daily probiotic, says Mashael Aljumaah, a doctoral student at the University of North Carolina at Chapel Hill (UNC) and North Carolina State University. In findings presented Monday at the American Society for Nutrition in Boston, Aljumaah and her colleagues at UNC and Kent State University in Ohio found that for older adults, a daily probiotic containing gut-friendly Lactobacillus rhamnosus helped improve mild cognitive impairment by resetting the imbalance in gut bacteria.

New research provides evidence that an individual’s health behaviors and outcomes are influenced by the genetic makeup of their romantic partner. The findings, published in Behavior Genetics, indicate that your partner’s genetic tendencies can lead to changes in your own weight, smoking habits, or alcohol consumption over time.
The researchers conducted this study to investigate how a person’s partner can affect their health. They aimed to explore the concept of social genetic effects, which refers to the impact of genetic factors in one person’s environment, such as their partner’s genotype, on their own phenotype (observable characteristics or traits).
“I was mainly interested in exploring the combination of social science and genetics,” explained study author Kasper Otten of Utrecht University. “It is evident that behavior is partly genetically influenced, but much of the social sciences does not deal with this biological fact.

Conclusions.
The vectorial role of bat flies should be checked by testing the same pathogen and bacterial organisms by collecting blood from host bats. This study is of great interest in the fields of disease ecology and public health owing to the bats’ potential to transmit pathogens to humans and/or livestock.
Covid is a bat bourne disease from such zoonotic transmission.
Background Bats are hosts for many ectoparasites and act as reservoirs for several infectious agents, some of which exhibit zoonotic potential. Here, species of bats and bat flies were identified and screened for microorganisms that could be mediated by bat flies. Methods Bat species were identified on the basis of their morphological characteristics. Bat flies associated with bat species were initially morphologically identified and further identified at the genus level by analyzing the cytochrome c oxidase subunit I gene. Different vector-borne pathogens and endosymbionts were screened using PCR to assess all possible relationships among bats, parasitic bat flies, and their associated organisms. Results Seventy-four bat flies were collected from 198 bats; 66 of these belonged to Nycteribiidae and eight to Streblidae families.

Ear infections in babies and toddlers are extremely common. In fact, according to the National Institutes of Health, five out of six children will experience an ear infection before their third birthday.
“Many parents are concerned that an ear infection will affect their child’s hearing irreversibly—or that an ear infection will go undetected and untreated,” says David Tunkel, M.D., Johns Hopkins Medicine pediatric otolaryngologist (ENT). “The good news is that most ear infections go away on their own, and those that don’t are typically easy to treat.”
Ear infections happen when there is inflammation— usually from trapped bacteria—in the middle ear, the part of the ear connects to the back of the nose and throat. The most common type of ear infection is otitis media, which results when fluid builds up behind the eardrum and parts of the middle ear become infected and swollen.
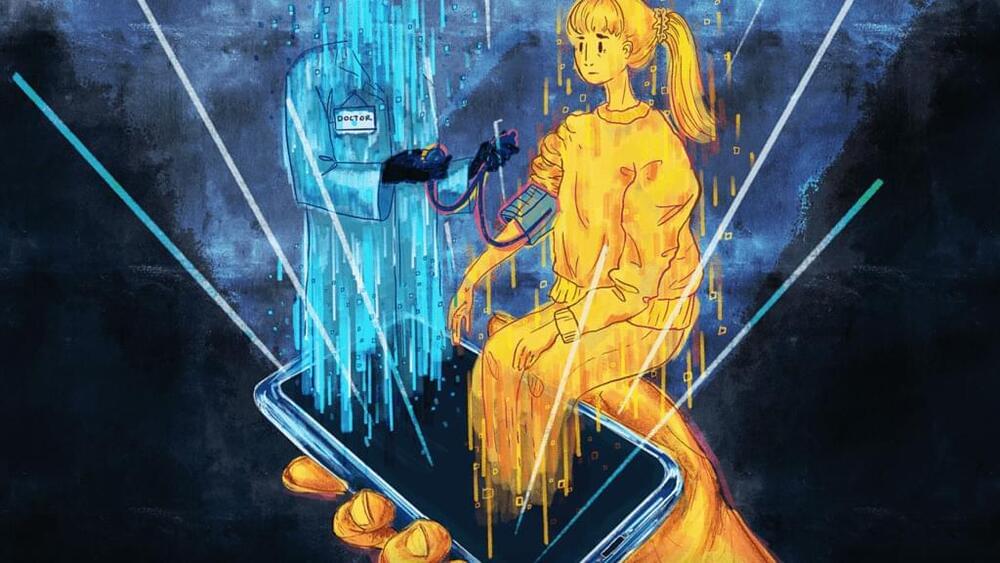
Since I was going to become a Dr before my TBI, or a scientist but there’s this and some devices and apps are pretty accurate. Like Samsung and Apple. Now there’s the Google Pixel, the Pixel watch and of course Fitbit and more.
The same devices used to take selfies and type out tweets are being repurposed and commercialized for quick access to information needed for monitoring a patient’s health. A fingertip pressed against a phone’s camera lens can measure a heart rate. The microphone, kept by the bedside, can screen for sleep apnea. Even the speaker is being tapped, to monitor breathing using sonar technology. Smartphones as medical devices could be the next big thing.
In the best of this new world, the data is conveyed remotely to a medical professional for the convenience and comfort of the patient. Or, in some cases, to support a clinician without the need for costly hardware.
But using smartphones as diagnostic tools is a work in progress, experts say. Some doctors and their patients have found some real-world success in deploying the phone as a medical device. However, the overall potential remains unfulfilled and uncertain.
Is Program Manager, Advanced Research Projects Agency for Health (ARPA-H — https://arpa-h.gov/people/ross-uhrich/), which is focused on advancing high-potential, high-impact biomedical and health research that cannot be readily accomplished through traditional research or commercial activity, accelerating better health outcomes targeting society’s most challenging health problems.
Under the ARPA-H portfolio, Dr. Uhrich is responsible for the recently launched Novel Innovations for Tissue Regeneration in Osteoarthritis (NITRO — https://arpa-h.gov/engage/programs/nitro/) program which seeks to develop new ways of helping the human body repair its own joints, with the goal of revolutionizing treatment for osteoarthritis — a common and often very painful condition where bones and cartilage break down.
Dr. Uhrich joined ARPA-H in March 2023 from Walter Reed National Military Medical Center (WRNMMC) and the Uniformed Services University of the Health Sciences, where he worked as a board-certified oral and maxillofacial surgeon and assistant professor of surgery. In addition to these roles, he spent 12 years with the U.S. Navy, finishing his tenure as a Lieutenant Commander.
Throughout his career, Dr. Uhrich has cared for thousands of members of the U.S. Armed Forces at various healthcare facilities, including the USS Gerald R. Ford, Naval Health Clinic Quantico, and WRNMMC, and served as an oral and maxillofacial surgery consultant to Congress. He also treated patients at Charleston Area Medical Center, R Adams Cowley Shock Trauma Center, and Suburban Hospital.
Dr. Uhrich holds a doctorate in dental medicine from the University of Pennsylvania, an MBA from the University of Virginia, and completed his surgical residency at WRNMMC. He also has a Bachelor of Science in Biomedical Engineering from Yale University.