Bionic limbs, bionic arms, bionic legs, prosthetic limbs, prosthetic arms, prosthetic legs, artificial limbs, artificial arms, artificial legs, robotic limbs, robotic arms, robotic legs, advanced prosthetics, advanced bionics, neural prosthetics, neural interfaces, brain-computer interface, brain-machine interface, sensory feedback prosthetics, touch-sensitive prosthetics, feeling prosthetics, prosthetics with sensation, prosthetics with touch, prosthetics with feeling, prosthetics with feedback, prosthetics with sensors, prosthetics with AI, prosthetics with machine learning, prosthetics with robotics, prosthetics with neural networks, prosthetics with brain control, prosthetics with mind control, prosthetics with thought control, prosthetics with nerve control, prosthetics with muscle control, prosthetics with EMG, prosthetics with EEG, prosthetics with TMR, prosthetics with osseointegration, prosthetics with myoelectric control, prosthetics with pattern recognition, prosthetics with haptics, prosthetics with vibration feedback, prosthetics with pressure sensors, prosthetics with temperature sensors, prosthetics with force sensors, prosthetics with motion sensors, prosthetics with position sensors, prosthetics with tactile sensors, prosthetics with kinesthetic feedback, prosthetics with proprioception, prosthetics with sensory substitution, prosthetics with sensory augmentation, prosthetics with sensory restoration, prosthetics with sensory integration, prosthetics with sensory encoding, prosthetics with sensory decoding, prosthetics with sensory stimulation, prosthetics with sensory perception, prosthetics with sensory experience, prosthetics with sensory illusion, prosthetics with sensory reality, prosthetics with sensory feedback loop, prosthetics with sensory feedback system, prosthetics with sensory feedback technology, prosthetics with sensory feedback device, prosthetics with sensory feedback mechanism, prosthetics with sensory feedback method, bionic limb technology, advanced prosthetic arms, robotic limb advancements, neural-controlled prosthetics, sensory feedback in prosthetics, touch-sensitive bionic limbs, brain-machine interface prosthetics, AI-powered prosthetic limbs, next-gen prosthetics, prosthetics with real sensation, smart prosthetic technology, haptic feedback prosthetics, nerve-integrated bionic limbs, mind-controlled prosthetics, future of prosthetic limbs, prosthetic limbs with touch, innovative prosthetic designs, cutting-edge bionic arms, prosthetics with sensory input, advanced limb replacement, intelligent prosthetic systems, prosthetic limbs with AI, sensory-enabled prosthetics, high-tech prosthetic limbs, prosthetics with neural feedback, robotic prosthetics with touch, advanced bionic limb systems, prosthetic limbs with real feel, smart bionic limb technology, prosthetics with brain interface, next-generation prosthetic limbs, prosthetics with sensory technology, AI-integrated prosthetic limbs, prosthetics with real-time feedback, advanced prosthetic limb control, prosthetics with tactile feedback, intelligent bionic limb systems, prosthetics with sensory integration, prosthetic limbs with neural control, advanced prosthetic limb technology, prosthetics with sensory enhancement, smart prosthetic limb systems, prosthetics with touch feedback, AI-driven prosthetic limbs, prosthetics with real sensation technology, advanced bionic limb control, prosthetics with sensory capabilities, intelligent prosthetic limb technology, prosthetics with tactile sensation, next-gen bionic limb systems, prosthetics with neural integration, smart prosthetic limb control, prosthetics with sensory feedback systems, advanced prosthetic limb designs, prosthetics with touch-sensitive technology, AI-powered bionic limbs, prosthetics with real-time sensory feedback, intelligent bionic limb control, prosthetics with sensory response, advanced prosthetic limb interfaces, prosthetics with tactile response, smart bionic limb control, prosthetics with sensory feedback integration, AI-integrated bionic limbs, prosthetics with real-time touch feedback, advanced prosthetic limb systems, prosthetics with sensory feedback technology, intelligent prosthetic limb systems, prosthetics with tactile feedback integration, next-gen prosthetic limb technology, prosthetics with sensory feedback mechanisms, synthetic limbs with emotion, AI in prosthetic development, robotic arms with brain control, feeling-enabled prosthetic arms, bionic sense of touch, real-time neural prosthetics, prosthetic limbs that feel pain, emotion-sensing bionic limbs, tactile bionic limb feedback, smart limbs with sensory feedback, neuroprosthetics with AI, feeling through robotic hands, human-machine sensory fusion, emotional robotics prosthetics, pain-sensing artificial limbs, robotic prosthetics with emotion, neural feedback robotic limbs, brain-connected prosthetic systems, adaptive robotic prosthetic, future prosthetics with emotions.
Category: cyborgs – Page 8



Tilly’s bionic hand can crawl around on its own
19-year-old Instagram influencer Tilly Lockey has been at the forefront of prosthetic innovation with UK-base…

First ‘smart,’ wearable, pediatric soft exoskeleton provides mobility for children with motor difficulties
Just one look at the next-generation lightweight, soft exoskeleton for children with cerebral palsy reveals the powerful role technology can play in solving global challenges and improving lives.
Built to help children walk, MyoStep addresses motor impairments that severely restrict children’s participation in physical activities, self-care and academic pursuits, leading to developmental delays, social isolation and reduced self-esteem. It is lightweight, discreet, made of smart materials and wearable technology, and tailored to fit seamlessly into the lives of children and their families.
The MyoStep soft exoskeleton is introduced in IEEE Electron Devices Magazine by a team from the NSF UH Building Reliable Advances and Innovation in Neurotechnology (BRAIN) Center, an Industry–University Cooperative Research Center (IUCRC) and TIRR Memorial Hermann.
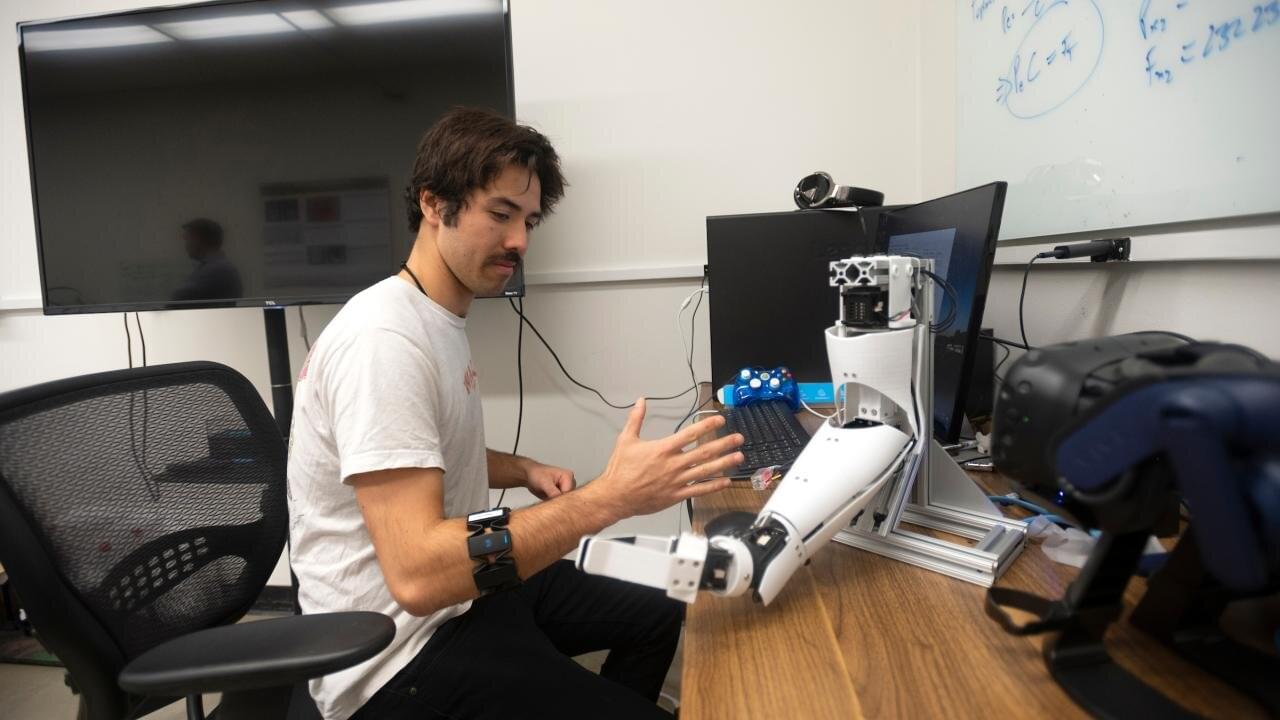
Combining electrical and force signals boosts prosthetic hand accuracy
Combining two different kinds of signals could help engineers build prosthetic limbs that better reproduce natural movements, according to a new study from the University of California, Davis. The work, published April 10 in PLOS One, shows that a combination of electromyography and force myography is more accurate at predicting hand movements than either method by itself.
The Rise of Cyborgs: Merging Man with Machine | Terrifying Future of Human Augmentation
Human cyborgs are individuals who integrate advanced technology into their bodies, enhancing their physical or cognitive abilities. This fusion of man and machine blurs the line between science fiction and reality, raising questions about the future of humanity, ethics, and the limits of human potential. From bionic limbs to brain-computer interfaces, cyborg technology is rapidly evolving, pushing us closer to a world where humans and machines become one.
Shocking transformation, futuristic nightmare, beyond human limits, man merges with machine, terrifying reality, future is now, ultimate evolution, secret experiments exposed, technology gone too far, sci-fi turns real, mind-blowing upgrade, science fiction no more, unstoppable machine man, breaking human boundaries, dark future ahead, human cyborgs, cyborg technology, cyborg implants, cyborg augmentation, cyborg evolution, cyborg future, cyborg innovations, cyborg advancements, cyborg ethics, cyborg integration, cyborg society, cyborg culture, cyborg development, cyborg research, cyborg science, cyborg engineering, cyborg design, cyborg applications, cyborg trends, cyborg news, cyborg updates, cyborg breakthroughs, cyborg discoveries, cyborg implants, bionic limbs, neural interfaces, prosthetic enhancements, biohacking, cybernetics, exoskeletons, brain-computer interfaces, robotic prosthetics, augmented humans, wearable technology, artificial organs, human augmentation, smart prosthetics, neuroprosthetics, biomechatronics, implantable devices, synthetic biology, transhumanism, bioengineering, nanotechnology, genetic engineering, bioinformatics, artificial intelligence, machine learning, robotics, automation, virtual reality, augmented reality, mixed reality, haptic feedback, sensory augmentation, cognitive enhancement, biofeedback, neurofeedback, brain mapping, neural networks, deep learning, biotechnology, regenerative medicine, tissue engineering, stem cells, gene therapy, personalized medicine, precision medicine, biomedical engineering, medical devices, health tech, digital health, telemedicine, eHealth, mHealth, health informatics, wearable sensors, fitness trackers, smartwatches, health monitoring, remote monitoring, patient engagement, health apps, health data, electronic health records, health analytics, health AI, medical robotics, surgical robots, rehabilitation robotics, assistive technology, disability tech, inclusive design, universal design, accessibility, adaptive technology, human-machine interaction, human-computer interaction, user experience, user interface, UX design, UI design, interaction design, design thinking, product design, industrial design, innovation, technology trends, future tech, emerging technologies, disruptive technologies, tech startups, tech entrepreneurship, venture capital, startup ecosystem, tech innovation, research and development, R&D, scientific research, science and technology, STEM, engineering, applied sciences, interdisciplinary research, academic research, scholarly articles, peer-reviewed journals, conferences, symposiums, workshops, seminars, webinars, online courses, e-learning, MOOCs, professional development, continuing education, certifications, credentials, skills development, career advancement, job market, employment trends, workforce development, labor market, gig economy, freelancing, remote work, telecommuting, digital nomads, coworking spaces, collaboration tools, project management, productivity tools, time management, work-life balance, mental health, wellness, self-care, mindfulness, meditation, stress management, resilience, personal growth, self-improvement, life coaching, goal setting, motivation, inspiration, success stories, case studies, testimonials, reviews, ratings, recommendations, referrals, networking, professional associations, industry groups, online communities, forums, discussion boards, social media, content creation, blogging, vlogging, podcasting, video production, photography, graphic design, animation, illustration, creative arts, performing arts, visual arts, music, literature, film, television, entertainment, media, journalism, news, reporting, storytelling, narrative, communication, public speaking, presentations, persuasion, negotiation, leadership, management, entrepreneurship, business, marketing, advertising, branding, public relations, sales, customer service, client relations, customer experience, market research, consumer behavior, demographics, psychographics, target audience, niche markets, segmentation, positioning, differentiation, competitive analysis, SWOT analysis, strategic planning, business development, growth strategies, scalability, sustainability, corporate social responsibility, ethics, compliance, governance, risk management, crisis management, change management, organizational behavior, corporate culture, diversity and inclusion, team building, collaboration, innovation management, knowledge management, intellectual property, patents, trademarks, copyrights.
Ultra-Strong Artificial Muscles Made From Carbon Nanotubes
In order to showcase ultra-strong artificial muscles, Ray Baughman from the University of Texas at Dallas and his colleagues built a catapult.
The scientists published their findings in the journal Science. The device contains yarns similar in diameter to human hair, spun from carbon nanotubes and soaked in paraffin wax. When a current is passed through the yarn, the wax heats up and expands. As the yarn swells, its particular helical weave causes it to shorten, and the muscle contracts. As it cools, the yarn relaxes and returns to its original length. When coiled lightly or heated to high enough temperatures, wax-free yarns behave in the same fashion.
The torque produced by the twisting and untwisting of the yarns is sufficient to power a miniature catapult. The yarn can haul 200 times the weight that a natural muscle of the same size can, and generates more torque than a large electric motor if compared by weight. Currently, the available manufacturing techniques have limited the weight of the yarn. They can make yarn that lifts up 50 grams. That doesn’t sound like much, but researchers have shown the nanotube yarns lifting loads as much as 50,000 times greater than their own weight.
Gold Nanoparticles Could Restore Vision in People with AMD
Could a tiny dose of gold restore sight? Researchers at Brown University have developed a groundbreaking retinal prosthesis using gold nanoparticles and infrared light to bypass damaged photoreceptors in retinal disorders like macular degeneration.
This minimally invasive method successfully activated the visual system in mice, offering promising early evidence for future clinical applications. Learn how this innovative fusion of nanotechnology and neuroscience could revolutionize treatment for millions suffering from vision loss.
#vision #visionloss #neuroscience #science