Rates of kidney stones are on the rise in the United States and around the world. Type 2 diabetes is associated with increased risk of kidney stones, but some forms of treatment for this condition may also have the benefit of lowering risk of kidney stones.
In a study led by investigators from Mass General Brigham, researchers found that there was an association between the use of sodium-glucose contratransporter 2 (SGLT2) inhibitors and a lower risk of developing kidney stones. Their findings are reported in JAMA Internal Medicine.
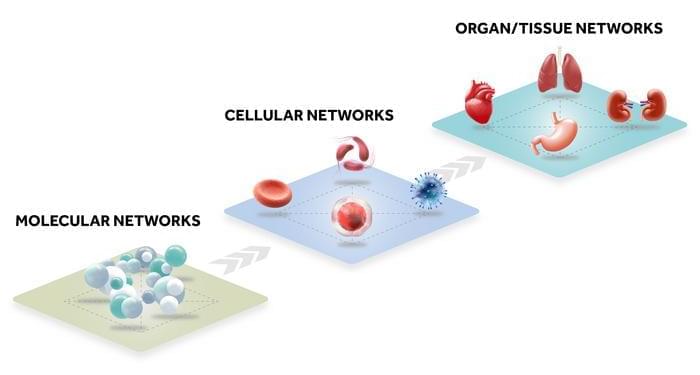
Researchers from Brigham and Women’s Hospital and Massachusetts General Hospital worked together to conduct the analysis. The study included data from three nationwide databases of patients with type 2 diabetes who were seen in routine clinical practice. The team analyzed information from 716,406 adults with type 2 diabetes who had started taking an SGLT2 inhibitor or two other classes of diabetes medications known as GLP1 receptor agonists or dipeptidyl peptidase 4 (DPP4) inhibitors.