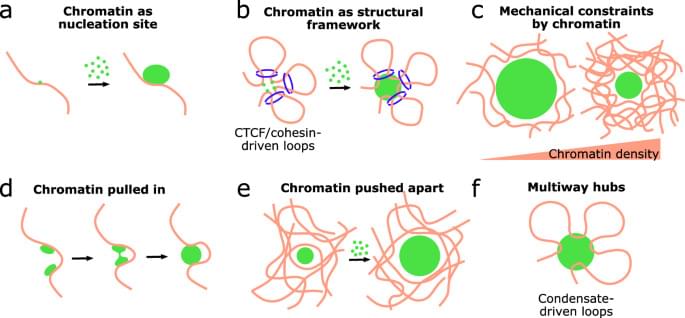
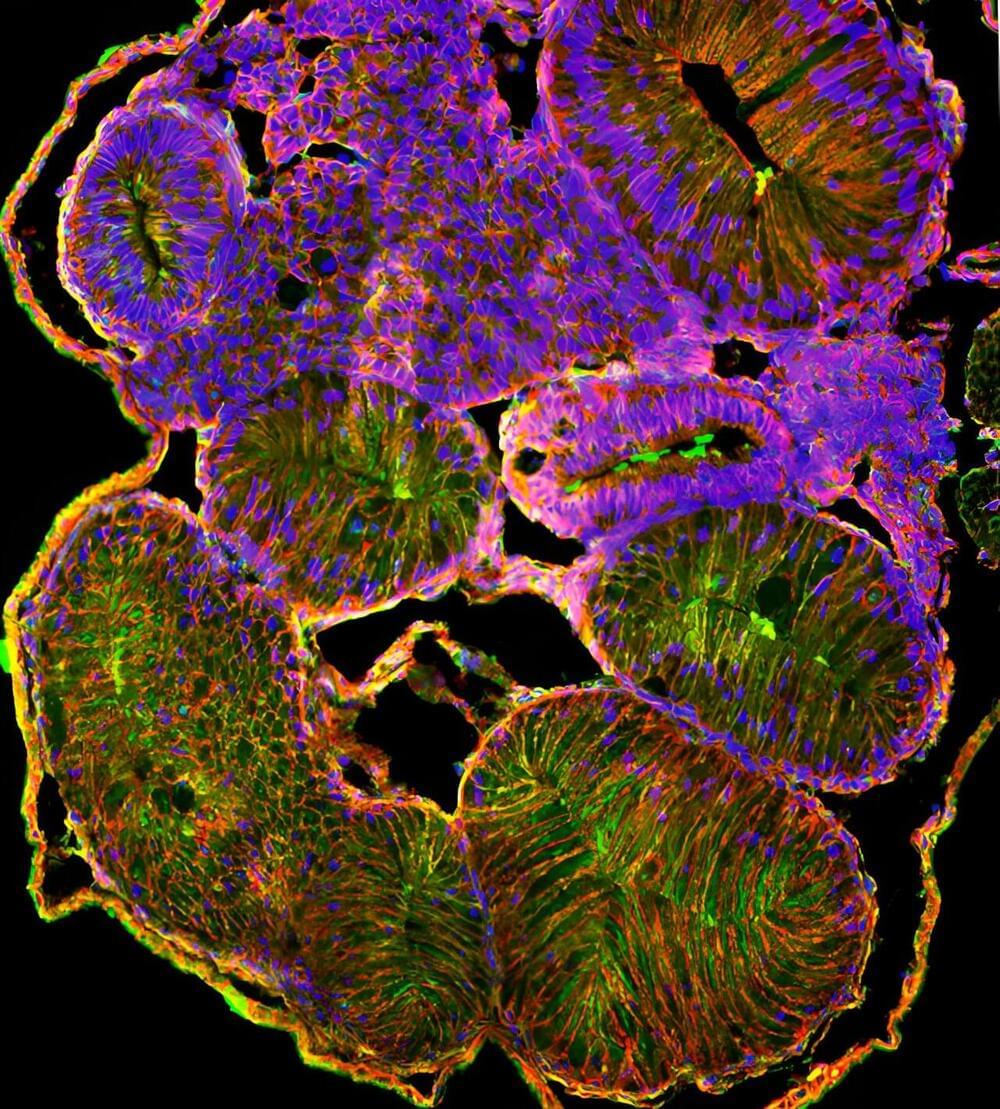
Genetic Engineering and DNA alteration is an emerging technology with huge ramifications in the future, including potentially altering the DNA of adult humans, not just embryos or plants \& animals.
Try Dashlane here: https://www.dashlane.com/isaacarthur.
Get 10% off now with my promo code: isaacarthur.
Visit our Website: http://www.isaacarthur.net.
Join Nebula: https://nebula.tv/videos/isaacarthur–…
Support us on Patreon: / isaacarthur.
Support us on Subscribestar: https://www.subscribestar.com/isaac-a…
Facebook Group: / 1583992725237264
Reddit: / isaacarthur.
Twitter: / isaac_a_arthur on Twitter and RT our future content.
SFIA Discord Server: / discord.
Listen or Download the audio of this episode from Soundcloud: Episode’s Audio-only version:
/ dna-manipulation-in-living-subjects.
Episode’s Narration-only version: / dna-manipulation-in-living-subjects-narrat…
Credits:
DNA Manipulation in Living Subjects (original title)
Genetically Altering Living Organisms.
Episode 227; Feb 27, 2020
Writers:
Isaac Arthur.
Editors: