Machine-learning system trained on millions of human audio clips shows promise for detecting COVID-19 and tuberculosis.


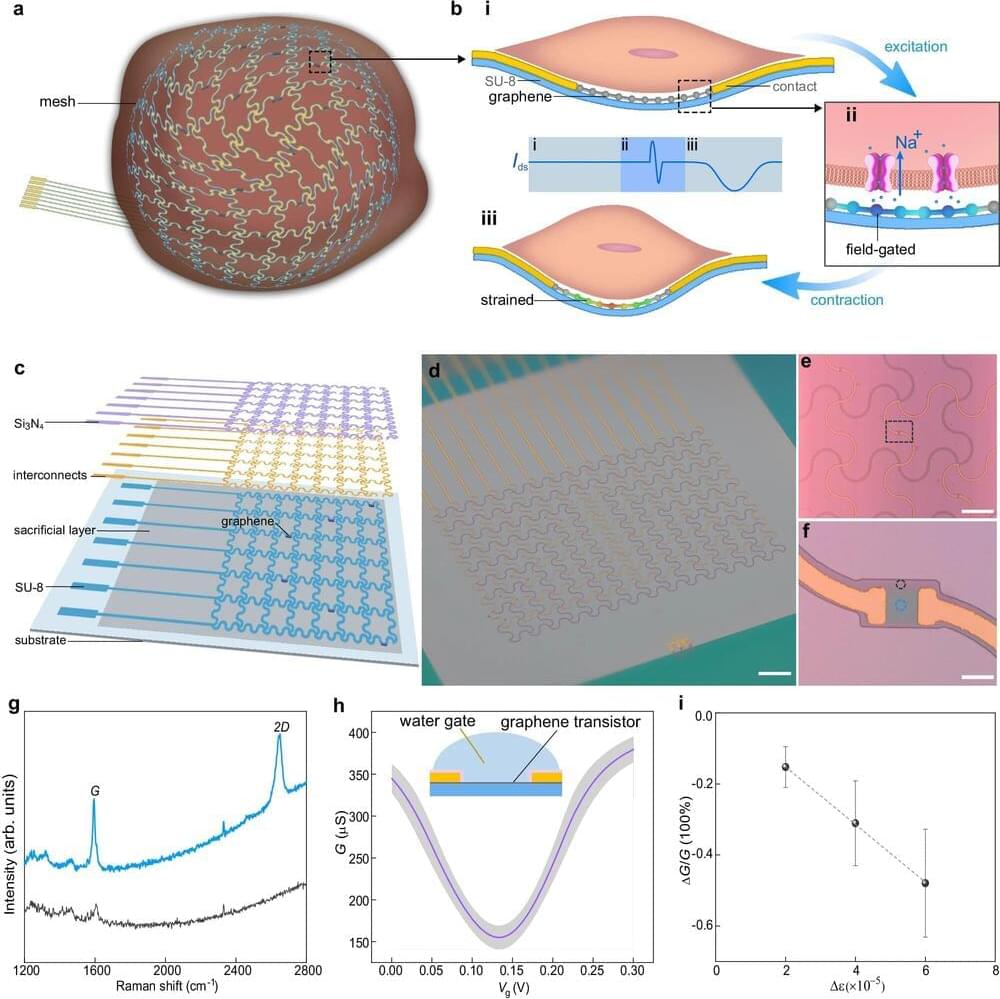
A team of engineers led by the University of Massachusetts Amherst and including colleagues from the Massachusetts Institute of Technology (MIT) recently announced in Nature Communications that they had successfully built a tissue-like bioelectronic mesh system integrated with an array of atom-thin graphene sensors that can simultaneously measure both the electrical signal and the physical movement of cells in lab-grown human cardiac tissue.
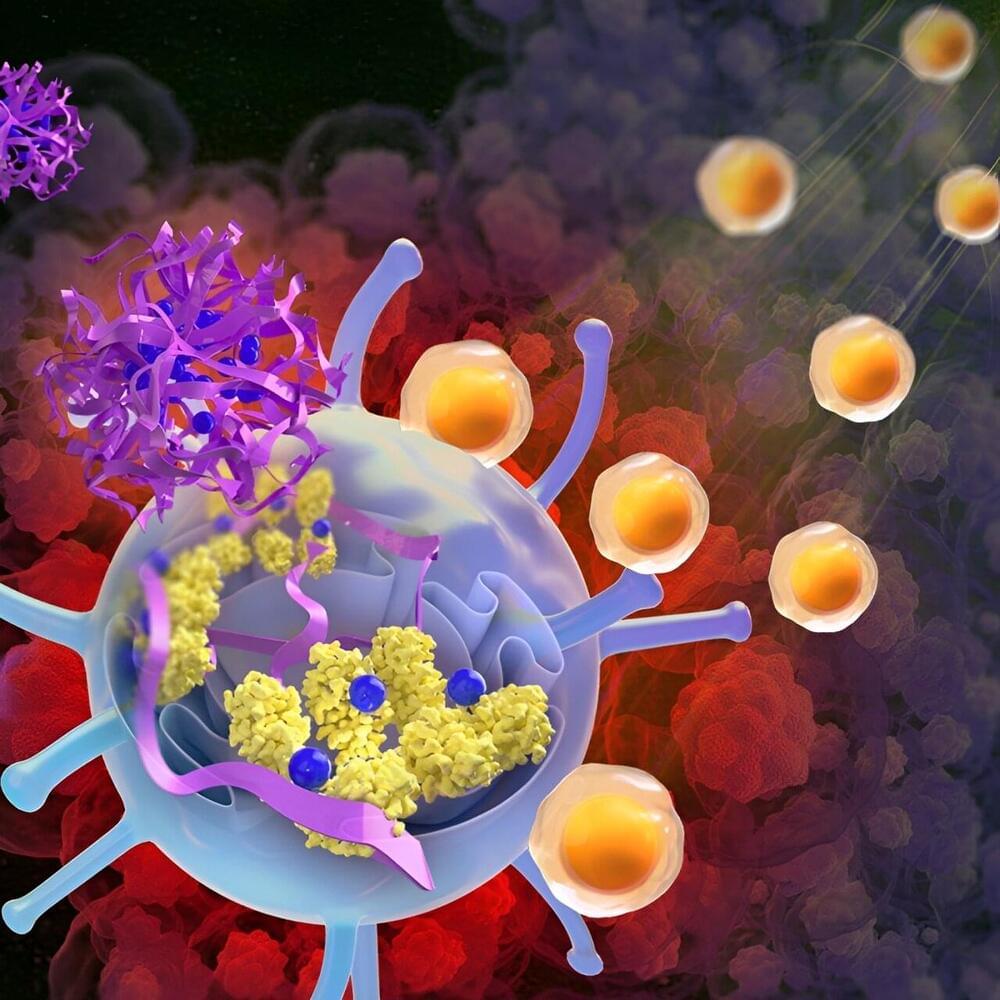
A nanoparticle-based therapy developed by UT Southwestern Medical Center scientists stimulated an immune pathway that eradicated tumors in mouse models of various cancer types. Their findings, published in Science Immunology, offer a new way to potentially harness the power of the body’s immune system against cancer.
Studies of brain network connectivity improved understanding on brain changes and adaptation in response to different pathologies. Synaptic plasticity, the ability of neurons to modify their connections, is involved in brain network remodeling following different types of brain damage (e.g., vascular, neurodegenerative, inflammatory). Although synaptic plasticity mechanisms have been extensively elucidated, how neural plasticity can shape network organization is far from being completely understood. Similarities existing between synaptic plasticity and principles governing brain network organization could be helpful to define brain network properties and reorganization profiles after damage. In this review, we discuss how different forms of synaptic plasticity, including homeostatic and anti-homeostatic mechanisms, could be directly involved in generating specific brain network characteristics. We propose that long-term potentiation could represent the neurophysiological basis for the formation of highly connected nodes (hubs). Conversely, homeostatic plasticity may contribute to stabilize network activity preventing poor and excessive connectivity in the peripheral nodes. In addition, synaptic plasticity dysfunction may drive brain network disruption in neuropsychiatric conditions such as Alzheimer’s disease and schizophrenia. Optimal network architecture, characterized by efficient information processing and resilience, and reorganization after damage strictly depend on the balance between these forms of plasticity.
Keywords: brain networks, connectivity, synaptic plasticity, Alzheimer’s disease (AD), schizophrenia, long-term potentiation (LTP), synaptic scaling, resting state functional MRI (rs-fMRI)
Our H+ friend Rob Wilkes alerted me to this today!
March 20 (Reuters) — Elon Musk’s brain-chip startup Neuralink livestreamed on Wednesday its first patient implanted with a chip using his mind to play online chess.
Noland Arbaugh, the 29-year-old patient who was paralyzed below the shoulder after a diving accident, played chess on his laptop and moved the cursor using the Neuralink device. The implant seeks to enable people to control a computer cursor or keyboard using only their thoughts.
Arbaugh had received an implant from the company in January and could control a computer mouse using his thoughts, Musk said last month.

Neuralink, Elon Musk ’s brain chip startup, released a video on Wednesday showing the company’s first patient using a laptop with just his mind.
The video, which was livestreamed on Neuralink’s account on X, showed 29-year-old Noland Arbaugh playing a game of chess on his laptop using Neuralink’s brain computer interface (BCI) technology. Arbaugh is paralyzed from the shoulders down due to what he describes as a “freak diving accident.”
“It’s all brain power there,” Arbaugh said, referring to his ability to use a mouse and keyboard unassisted. He later added, “Basically, it was like using the Force on the cursor and I could get it to move wherever I wanted.”

The immune system is comprised of two separate responses referred to as either innate or adaptive immunity. Both work in collaboration to elicit protection against anything the body encounters as ‘foreign’. In many cases foreign pathogens that enter the body are recognized by the innate immune system first which then activate adaptive immunity. The innate immune system uses many broad, non-specific cells to detect anything that might cause harm to the body. These cells initiate inflammation and the overall immune response. The adaptive immune system comes second and is more specific to the invading pathogen. Adaptive immune cells can not only help lyse or kill the invaders, but also generate cells to ‘remember’ that pathogen in the future. This is a common phenomenon that occurs when we overcome an illness and is known as immunological memory. Vaccine biology is based on this concept that we will generate ‘memory cells’ in response to attenuated viruses.
The study of immunity and how our body fights off disease is a progressively growing field. Currently, scientists know many of the key players that drive this immunological memory. However, researchers and physicians are working together to better understand this process and how to generate more effective treatments for various diseases. An exciting article in Nature, published by Dr. Francisco J. Quintana and others, demonstrate that a glial cell can generate immunological memory. Quintana, an investigator at Brigham and Women’s Hospital, and his team study different signaling pathways associated with immune activity to identify novel therapeutic treatments and biomarkers to measure treatment efficacy. The glial cell Quintana and his team found to aid in immunity is known as an astrocyte, which is a key cell within the central nervous system (CNS). Astrocytes help promote synapse formation, clear excess neurotransmitters, and maintain the blood-brain barrier.
For the first time astrocytes have been connected to obtain memory-like properties and aid in immunity. The team used multiple models to demonstrate that astrocytes can remember previous interactions with immune cells. Not only did this function improve response time to infection but induced a stronger immune response when re-exposed to the same disease. Due to similarities in memory formation, Quintana and others refer to this process as ‘astrocyte immune memory’. Interestingly, due to astrocytes long lifespan, these cells could provide insight into chronic neurologic disorders.