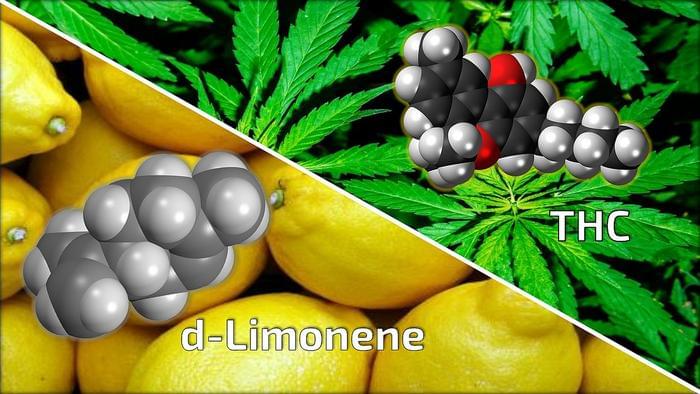
“This study is a first step in uncovering how we can mitigate risks of THC when used in medicine, and also is targeted at making cannabis safer for the general, non-therapeutic consumer,” said Dr. Tory Spindle.
Can cannabis be modified to decrease certain side effects, specifically anxiety, that is caused by tetrahydrocannabinol (THC)? This is what a recent study published in Drug and Alcohol Dependence hopes to address as a team of researchers led by the Johns Hopkins University School of Medicine investigated whether adding d-limonene, which is a known cannabis oil, to THC could help alleviate common feelings of anxiety or paranoia that cannabis users traditionally experience. This study holds the potential to help improve medicinal cannabis while decreasing risks to users of recreational cannabis, as well.
For the study, the researchers enlisted 20 healthy adult participants with an average age of 26 years old who completed 10 six-hour sessions involving them using vaporized THC alone (15 mg or 30 mg), vaporized d-limonene alone (1 mg or 5 mg), both together, and finally a placebo. The sessions were double-blinded, meaning both the researchers and participants were unaware who was vaporizing which sample.
While all 20 participated in nine sessions, 12 participants conducted the tenth session comprised of the higher dose of THC and an even higher dose of d-limonene at 15 mg. The goal of the sessions was to ascertain the overall drug effects, specifically vital signs, mood, and cognitive functions, along with blood and urine samples during and after each session to measure THC and d-limonene levels.